The NHS interview questions is a critical milestone for anyone aiming to start or advance their careers in the UK. It’s not just a test of your clinical knowledge—it’s a holistic evaluation of your competencies, communication skills, ethical reasoning, and alignment with NHS values like compassion and teamwork.
This expanded guide will help you tackle every aspect of the NHS interview with confidence, including competency-based interview questions and answers. We’ll dive deeply into common question categories, explore effective frameworks including the STAR and CAMP methods, and provide actionable tips to ace your interview.
Whether you’re applying for a junior doctor post or a Band 6 nurse position, this will help you prepare with confidence.
Types of NHS Interview Questions
You’ll usually encounter these 4 formats:
1. NHS Values-Based Interview Questions
These assess how well you align with NHS core values (from the NHS Constitution). Example questions:
- “Describe a time you showed compassion at work.”
- “How do you ensure respect and dignity in your clinical practice?”
2. Competency-Based NHS Interview Questions
Used for Band 5 and Band 6 interviews especially. Focus on your ability to:
- Work under pressure
- Communicate effectively
- Lead teams
Example:
“Tell us about a time you dealt with a difficult colleague.”
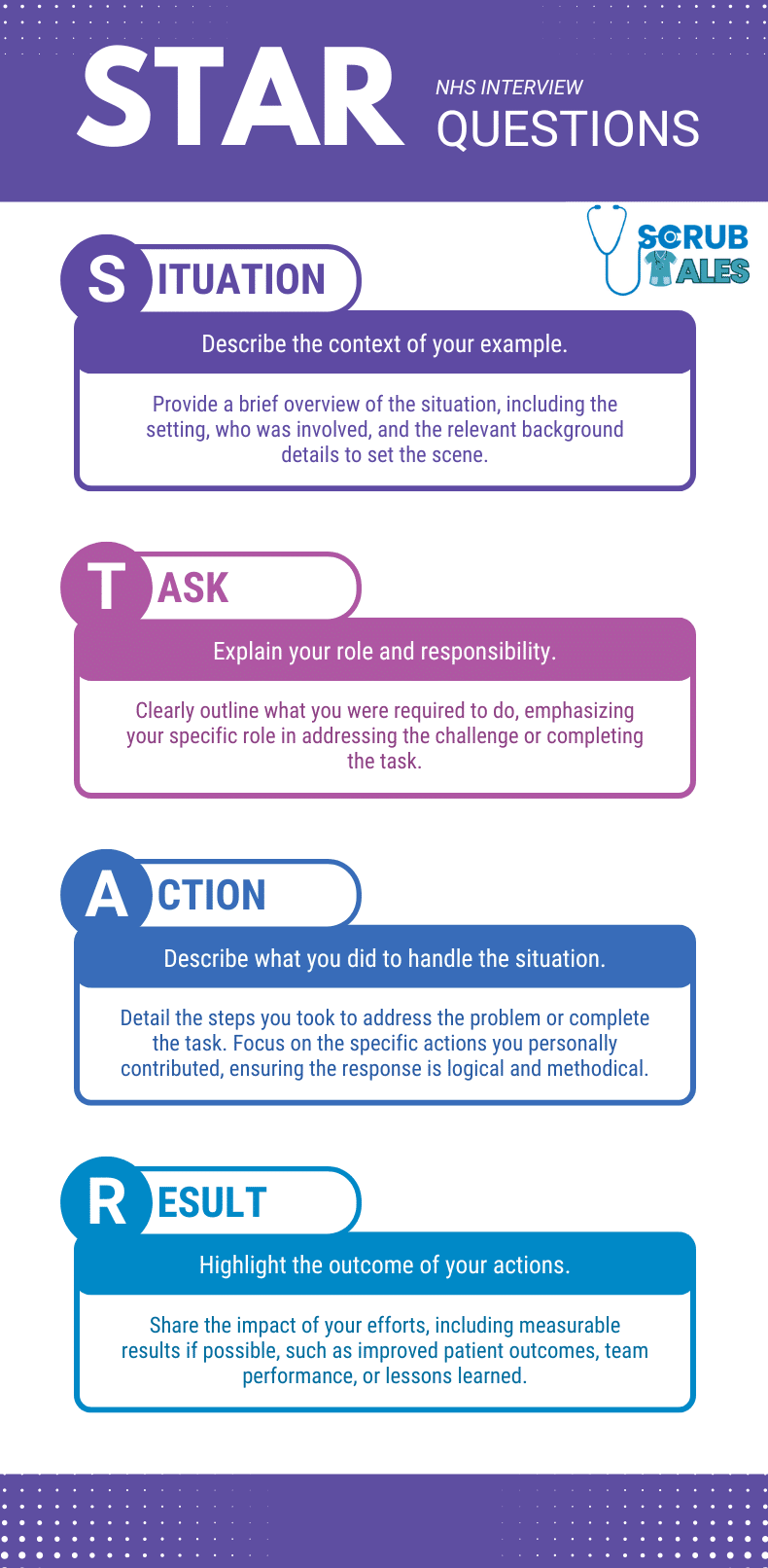
Use the STAR method: Situation → Task → Action → Result.
3. Clinical Scenario Questions (for junior doctors)
Expect questions like:
- “What would you do if a patient collapses on the ward?”
- “How do you manage a deteriorating patient?”
Frameworks like ABCDE or SBARR help structure your answer.
4. Governance & Ethical Scenarios
These are crucial for IMG doctors and Band 6 applicants:
- “What would you do if you saw a colleague not washing their hands?”
- “You made a prescribing error—what next?”
Use frameworks like SPIES or Duties of a Doctor (GMC).
Why NHS Interviews Are Unique
NHS interviews are highly structured, competency-based, and focused on fairness, and the complexity of NHS interview questions is variable. A competency-based interview is a structured method used by hiring managers to assess candidates’ key competencies and specific skills relevant to the role.
In these interviews, candidates are assessed through competency-based interview questions designed to evaluate their suitability for the NHS. They are designed to test your ability to meet the clinical, ethical, and communication demands of the role.
If you are the lucky ones to land an interview in the current saturation, then this post is for you. If not, you should probably check out our guides on Trac Job Application Guide with tempaltes for doctors.
![[2025] Competency-Based NHS Interview Questions and Answers 1 Funny meme 1](https://scrubtales.co.uk/wp-content/uploads/Funny-meme-1.webp)
Key Features
- Structured Questions: Every interview question is asked by an interviewer who evaluates your response based on pre-set criteria to assess specific competencies.
- Scenario-Based Assessments: Clinical scenarios are designed to evaluate decision-making under pressure.
- Focus on NHS Core Values: Compassion, teamwork, and integrity are integral to the evaluation process.
- Evidence-Based Practice: Familiarity with UK guidelines, such as NICE and the GMC’s Good Medical Practice, is expected.
Preparing for the NHS Interview Questions
A. Research the Role and Trust
Start by thoroughly understanding the job description and the trust you’re applying to. It depends where you applied the job, if on TRAC jobs, you must read the job description PDF file first.
Focus on:
- Job Description: Read it thoroughly and make points as to what the role is, what your duties will be, which specialty you will be working in, what rotations are there, on-calls, clerking and post-take, etc. This gives you a good idea of what the clinical questions can be and what guidelines can be followed.
- Speciality Needs: Learn about the trust’s priorities and unique patient demographics.
- Trust Culture: Familiarise yourself with the trust’s values, mission, and achievements. (Trust values are a must know)
B. Portfolio Preparation
Your portfolio should reflect your experience, skills, and accomplishments. Include:
- Certificates: Highlight courses, CPD activities, and qualifications.
- Research and Audits: Showcase completed projects with measurable outcomes.
- Evidence of Leadership: Include instances where you’ve led or managed initiatives.
C. Study Relevant Guidelines
- Oxford Handbook – If you are applying for a junior doctor post, this is highly recommended. Please review all the major flowcharts and be prepared to answer questions about them.
- Here is the Recommended Book for NHS Interview Questions with Answers for clinical part: BUY OXFORD Handbook
- NICE Guidelines: Familiarize yourself with protocols for common clinical scenarios.
- GMC Guidance: Understand key principles from documents like Good Medical Practice.
- Self Notes: These are the best in my opinion. Use the short notes you created while preparing for exams, whether PLAB, MSRA or MRCS.
3. The Structure of NHS Interview
A. Types of Interview Formats
| Interview Format | Description |
|---|---|
| Panel Interviews | A standard format involving 2-4 interviewers, such as consultants, senior clinicians, or HR representatives. These interviews cover clinical scenarios, ethical questions, and communication skills. |
| Station-Based Interviews | Common for speciality roles. Candidates rotate through multiple stations testing various competencies, such as clinical decision-making, teaching ability, and communication skills. |
| Virtual Interviews | Conducted online, requiring strong technical preparation. Candidates must ensure stable internet, proper lighting, and a professional background to make a good impression. |
4. NHS Interview Question Categories
NHS interviews are structured to assess a variety of competencies. They often include competency-based interview questions and competency-based questions, which are designed to evaluate your ability to answer effectively and relate your experiences to the key competencies required for the role.
Answering competency-based questions effectively provides interviewers with valuable insight into your skills, thinking process, and suitability for the position. Here’s a detailed breakdown of each question category, along with tips and examples for success.
But before we start, let’s have a quick look at what common frameworks are used to answer these questions asked in NHS interviews:
Frameworks for Answering NHS Interview Questions
The NHS interview process often requires structured and well-organised answers to clinical, behavioural, ethical, and motivation-based questions. Using frameworks like CAMP, STAR, SPIES, and ABCDE ensures clarity and completeness in your responses.
The STAR technique, also known as the STAR method, is crucial for clearly describing your actions and results in competency-based interview questions. When using these frameworks, always give an example to illustrate your competencies.
| Framework | Use Case | Steps/Components | Example Application |
|---|---|---|---|
| CAMP | Motivation and background questions |
|
“Why do you want to work in the NHS?” |
| STAR | Behavioral and situational questions |
|
“Describe a time you handled a conflict with a colleague.” |
| SPIES | Ethical and governance questions |
|
“What would you do if a colleague arrived intoxicated at work?” |
| ABCDE | Clinical scenario questions |
|
“A patient presents with severe chest pain. What’s your approach?” |
- CAMP: Best for motivation and background questions, this framework helps align your career aspirations with NHS values while showcasing your clinical, academic, and leadership potential.
- STAR: Designed for behavioural and situational questions, the STAR technique ensures a structured, impactful answer by focusing on the context, your role, describing your actions, and the outcome. Always give an example to highlight your relevant skills and experiences.
- SPIES: Ideal for ethical dilemmas, SPIES emphasizes patient safety, proper escalation, and providing support while addressing governance issues.
- ABCDE: Used in clinical scenarios, ABCDE ensures a systematic approach to assessing and managing patient conditions by addressing airway, breathing, circulation, disability, and exposure.
Walk Us Through Your CV
This needs to be delivered in 3 minutes maximum. Mostly, it ends in less than a minute, given the number of applications that are interviewed these days of NHS saturation.
You should use a CAMP structure. When walking through your CV, consider including an example of a time when you demonstrated a key competency, such as problem-solving or adaptability, using the STAR format. If you have delivered the best presentation in a team project or similar context, mention this as an achievement to highlight your communication and teamwork skills.
Also, reflect on situations where you might have approached things differently and share what you learned from those experiences. Even if you are not able to finish half of it, do not be disheartened. The idea is to inform the panel that you are prepared, and trust me, they can identify it once you use the proper structure.
![[2025] Competency-Based NHS Interview Questions and Answers 3 Funny meme 2](https://scrubtales.co.uk/wp-content/uploads/Funny-meme-2.webp)
How to Write a CV Using the CAMP Framework
When writing a CV for an NHS role, it’s essential to focus on these four key areas:
- Clinical (Qualifications and Experience)
- Begin with your medical qualifications (e.g., MBBS, MRCP) and clinical training.
- Highlight your relevant experience, including specialities, procedures, and patient populations you’ve worked with.
- Mention specific competencies, such as managing emergencies, working in multidisciplinary teams, or adhering to NICE guidelines.
- Clearly state your key skills relevant to the NHS role, such as effective communication, clinical decision-making, and teamwork, to demonstrate your strengths in essential areas.
- Academic (CPD and Research)
- Include Continuing Professional Development (CPD) courses, certifications, or workshops you’ve attended.
- Mention any research projects, publications, or presentations, emphasising their relevance to the role.
- Focus on how these experiences have enhanced your knowledge and clinical practice.
- Highlight key skills developed through academic work, such as critical appraisal, data analysis, and evidence-based practice.
- Management (QIP and Teaching)
- Highlight your involvement in Quality Improvement Projects (QIP), audits, or leadership roles.
- Showcase your teaching experience, such as mentoring junior doctors, leading sessions, or creating educational materials.
- Include examples of initiatives where you’ve improved workflows or patient care.
- Personal (Hobbies and Future Plans)
- Add a personal touch by including hobbies or activities that demonstrate balance and resilience.
- Outline your career aspirations, showing your alignment with NHS values and the role you’re applying for.
- Briefly mention how your experiences and skills demonstrate your suitability for the position, emphasising your commitment and fit for the NHS environment.
Sample Walk Us Through Your CV Template
Below is a template for this section of NHS Interview Questions; however, I hardly believe I could recite 20% of it in the interview. The idea is to create a personalised version and practice to complete it in less than 3 minutes.
- I qualified in 2017, following which I completed a one-year structured foundation programme that included rotations in surgical and medical specialities. From 2018, I worked a total of 3 years as SHO in Internal Medicine, Gastroenterology, Respiratory Medicine and General Surgery. I have completed my PLAB part 1 and 2 exams and hold full GMC registration with a license to practice.
- Currently, I am undertaking a Clinical Attachment in the Colorectal Surgery Department at Basingstoke and Northern Hampshire NHS Foundation Trust, under the guidance of Mr Francesco Di Fabio, a colorectal consultant.
- My primary responsibilities here involve shadowing the SHO, FY1 and Consultant. I perform duties such as attending ward rounds, Colorectal as well as PMI MDTs, attending elective theatres and clinics, and joining on-call teams whenever necessary. I assist FY1s in clerking patients, identifying red flags, writing discharge letters, prescribing medications, ordering investigations and other tasks involved in patient care. We also hold informal teaching sessions, during which we discuss clinical scenarios and possible management plans for complex cases.
- Previously, while working as an SHO in India, I was exposed to various cases in respiratory medicine, general medicine, and general surgery, encompassing the elderly population as well. I often performed duties in different settings, such as acute medical unit, outpatient as well as diabetic clinics, wards, and Respiratory ITU during COVID-19 duties. I would say I am fairly exposed to several clinical cases such as DKA, ACS, Pneumonia, COPD, Asthma, COVID-19, DVT, TB and ILD. I have also managed cases such as anaphylaxis, pneumothorax, AKI, acute poisoning and road traffic accidents under supervision and contributed directly as a member of the team.
- I am competent in basic procedures, including adult IV cannulation, urinary catheterisation, and NGT insertion, as well as blood sampling, interpreting ABG, and performing basic investigations such as FBC, U&E, CXR, and ECG. Additionally, I am skilled in advanced procedures, including diagnostic lumbar puncture, Diagnostic and therapeutic Ascitic tap, and Femoral or Radial Artery puncture. I am also very proficient in systemic examination and CPR, and can deliver an engaging teaching session on the same topics. Apart from learning through experience as SHO, I have also undergone various training programmes for basic and advanced procedures to enhance my knowledge of these core skills further.
- For QIP, I completed QI Training at the Bronze level with the NHS and am currently helping one of the FY1s with her QIP. As for research, I do not have any publications to date, but I am seeking an opportunity, having completed “Improving Healthcare Through Clinical Research” by the NIHR and “Good Clinical Practice” by the NIDA Clinical Trials Network. Additionally, I am preparing a presentation on Pulmonary Embolism, which I plan to present at the Mortality and Morbidity meeting after consulting with my consultant.
- I am also enthusiastic about teaching, as I have held multiple informal training sessions with my juniors on topics such as the interpretation of CXR and ABG, and have received fantastic feedback on these sessions. I also completed Train the Healthcare Trainer by NHS Health Education England to hone my skills of teaching.
When I was writing this answer, it was a template for me. Of course, when answering, you should sound natural. Laugh a bit, joke around and be fluent with naturally.
Most of all, do not sound robotic for god sake.
A. Clinical Scenario NHS Interview Questions
Clinical scenario questions test your ability to assess, diagnose, and manage medical situations using evidence-based practices. These questions also evaluate your decision-making, prioritisation skills, and adherence to UK guidelines.
| Example Questions | Framework to Use |
|---|---|
| A patient presents with severe chest pain. What’s your approach? | ABCDE, NICE Guidelines |
| A child with a fever and rash is brought to A&E. How would you manage this case? | ABCDE |
| A patient is found unresponsive on the ward. What steps would you take? | Resuscitation Protocols |
Tips for Answering Clinical Scenario Questions in NHS Job Interview:
- Follow a Framework: Use structured frameworks like ABCDE or SBAR to organize your response.
- Highlight Patient Safety: Always prioritise immediate interventions that ensure safety.
- Reference UK Guidelines: Mention relevant guidelines like NICE, especially when discussing investigations or treatment.
- Incorporate Teamwork: Emphasize communication and collaboration with colleagues.
- Mention Relevant Projects: If you have led or participated in a project that improved clinical processes or patient care, briefly describe your role and the outcome to demonstrate your initiative and impact.
Sample Answer: “For a patient presenting with chest pain, I would begin with an ABCDE assessment. My priority would be to ensure the airway is clear and provide oxygen if needed. I would order an ECG and troponin levels to investigate a potential myocardial infarction. Following NICE guidelines, I’d administer aspirin and escalate to cardiology for PCI if indicated. I would also communicate with nursing staff and document my actions thoroughly.”
![[2025] Competency-Based NHS Interview Questions and Answers 4 Funny meme 3](https://scrubtales.co.uk/wp-content/uploads/Funny-meme-3.webp)
Clinical Scenario Questions Templates
1. A patient presents with severe chest pain. What’s your approach?
Answer:
“I would perform an ABCDE assessment to stabilize the patient. After ensuring the airway is clear and providing oxygen if needed, I would check breathing with auscultation and perform a bedside ECG. Based on NICE guidelines, I’d administer aspirin and nitroglycerin and escalate to cardiology for PCI. Clear documentation and communication with the team would be my priority.”
2. A child with fever and rash is brought to A&E. How would you manage this case?
Answer:
“I would suspect meningitis or a viral exanthem. Using ABCDE, I’d assess vitals, ensure hydration, and initiate antibiotics if meningitis is suspected. I’d inform paediatricians for further management and counsel the family.”
3. A patient is found unresponsive on the ward. What steps would you take?
Answer:
“Using the resuscitation protocol, I would call for help, check responsiveness, and begin CPR if needed. Simultaneously, I’d ensure airway patency and call the crash team.”
4. A patient reports dizziness and fainting episodes. How would you investigate?
Answer:
“I would focus on cardiovascular and neurological causes. Initial steps include ECG, orthostatic blood pressure measurements, and referral for Holter monitoring.”
5. A pregnant woman arrives with abdominal pain. What’s your approach?
Answer:
“After stabilising vitals, I’d conduct a focused history to rule out obstetric emergencies like ectopic pregnancy. Immediate referral to obstetrics would follow.”
6. A diabetic patient presents with DKA. How do you manage this?
Answer:
“I’d start with fluid resuscitation, administer insulin, and correct electrolyte imbalances per NICE guidelines. Continuous monitoring and team communication are key.”
7. A patient has severe shortness of breath and leg swelling. What would you do?
Answer:
“Suspecting heart failure or a pulmonary embolism, I’d start with oxygen, order BNP or D-dimer tests, and perform an echocardiogram.”
8. A patient is admitted with acute confusion and fever. What is your approach?
Answer:
“I’d suspect sepsis and initiate the sepsis six protocol: oxygen, antibiotics, IV fluids, and blood cultures.”
9. A child with head trauma has persistent vomiting. How would you proceed?
Answer:
“I’d stabilise the child, assess Glasgow Coma Scale, and refer urgently for a CT scan.”
10. A patient presents with suspected drug overdose. What’s your management plan?
Answer:
“I’d ensure ABC stability, administer activated charcoal if appropriate, and involve the toxicology team.”
B. Behavioral and Situational Questions
These NHS interview questions evaluate your past behaviour to predict your future behaviour in similar situations. They focus on how you manage interpersonal challenges, solve problems, and demonstrate leadership.
| Example Questions | Framework to Use |
|---|---|
| Tell us about a time you worked in a challenging team environment. | STAR Framework |
| Describe a situation where you went above and beyond for a patient. | STAR |
| How do you handle disagreements with colleagues? | STAR |
![[2025] Competency-Based NHS Interview Questions and Answers 5 Funny meme 4](https://scrubtales.co.uk/wp-content/uploads/Funny-meme-4.webp)
Tips for Answering Behavioral and Situational NHS Interview Questions:
- Be Specific: Use real examples from your experience.
- Follow the STAR Framework: Organise your response into Situation, Task, Action, and Result for clarity.
- Focus on Positives: Highlight the lessons learned and how the experience improved your skills.
- Demonstrate Managing Competing Priorities: Show how you effectively balanced competing priorities and managed your workload in a fast-paced environment.
Sample Answer: “In my previous role, a patient’s blood results were delayed, causing frustration among colleagues. As the team leader, I identified the bottleneck in the lab and arranged for expedited processing. Meanwhile, I kept the team updated and reassured the patient. The issue was resolved efficiently, and the lab implemented new protocols to prevent similar delays in the future. This experience reinforced the importance of communication and proactive problem-solving.”
Behavioral and Situational Questions Templates
1. Tell us about a time you resolved a conflict with a colleague.
Answer (STAR):
S: During a busy shift, a nurse felt overburdened with tasks. T: I was responsible for managing team dynamics. A: I privately discussed their concerns and reallocated tasks. R: The shift proceeded smoothly, and team morale improved.
2. Share a time you prioritized tasks under pressure.
Answer:
“During a medical emergency, I triaged patients, attending to the most critical first. This ensured optimal care despite limited resources.”
3. Can you provide an example of working with a difficult patient?
Answer:
“I once managed a patient who refused treatment. I explained the risks and benefits patiently, addressed their concerns, and eventually gained their trust.”
4. Describe a time you exceeded patient expectations.
Answer:
“I stayed late after my shift to arrange transport for a patient who couldn’t get home. This small act reassured them and their family.”
5. Tell us about a time you worked in a multidisciplinary team.
Answer:
“While handling a stroke case, I collaborated with nurses, radiologists, and physiotherapists. This teamwork ensured timely thrombolysis and excellent recovery.”
C. Ethical and Governance Questions
Ethical questions in NHS job interviews assess your understanding of professionalism, patient safety, and adherence to the GMC’s Good Medical Practice guidelines. They often involve complex dilemmas that require careful consideration.
These questions also help interviewers assess your potential future performance in challenging situations by evaluating how you might respond to ethical dilemmas.
| Example Questions | Framework to Use |
|---|---|
| What would you do if a colleague arrived intoxicated to work? | SPIES Framework |
| You notice a senior colleague making a clinical error. How would you handle it? | SPIES |
| How would you respond to a patient refusing treatment? | Ethical Principles (Autonomy, Beneficence, etc.) |
![[2025] Competency-Based NHS Interview Questions and Answers 7 Funny meme 5](https://scrubtales.co.uk/wp-content/uploads/Funny-meme-5.webp)
Tips for Answering Ethical Questions in NHS interviews:
- Follow Ethical Principles: Respect autonomy, prioritise beneficence, and balance non-maleficence with justice.
- Use the SPIES Framework to structure your response, ensuring a logical and professional approach.
- Demonstrate Integrity: Show your commitment to ethical standards and patient safety.
Sample Answer (Using SPIES): “If I noticed a colleague intoxicated at work, I would first discreetly confirm my observations (Seek Information). My priority would be patient safety, so I would ensure they are removed from clinical duties (Patient Safety). I would inform my supervisor and document the incident appropriately (Escalate). Finally, I would offer support to the colleague by directing them to occupational health services (Support).”
Ethical and Governance Questions Templates
1. What would you do if a colleague arrived intoxicated at work?
Answer (SPIES):
“I’d seek confirmation discreetly, prioritise patient safety by removing them from duties, escalate to a supervisor, and support them with occupational health referrals.”
2. How would you handle a senior colleague’s clinical error?
Answer:
“I’d document observations, discuss with them respectfully, and escalate if patient safety is compromised.”
3. A patient refuses life-saving treatment. What would you do?
Answer:
“I’d respect their autonomy, ensure they understand risks, and document the refusal after confirming mental capacity.”
4. How would you respond to a confidentiality breach?
Answer:
“I’d inform the colleague of the breach, escalate it, and ensure the patient is reassured about corrective actions.”
D. Background and Motivation Questions
Motivation NHS interview questions explore your reasons for pursuing a role in the NHS and your long-term career goals.
| Example Questions | Framework to Use |
|---|---|
| Why do you want to work in the NHS? | CAMP Framework |
| What are your career goals for the next five years? | Structured Plan |
| How does your background prepare you for this role? | Reflective Approach |
Tips for Answering Motivation Questions:
- Use the CAMP Framework:
- Clinical: Highlight opportunities for skill development.
- Academic: Mention your interest in teaching or research.
- Management: Discuss leadership aspirations.
- Personal: Align your goals with NHS values.
- Be Honest: Reflect on your journey and what draws you to the NHS.
- Show Passion: Let your enthusiasm for the role and organisation shine through.
- Demonstrate the Candidate’s Ability to Align with Company Goals: Show how your skills, values, and experiences match the NHS’s mission and how you can contribute to the company’s success.
Advice: Prepare thoughtful and authentic answers by researching the NHS’s values and goals, reflecting on your motivations, and practising how to demonstrate your candidate’s ability to contribute to the company. This advice will help you provide genuine responses that stand out in NHS interview questions.
Sample Answer: “I am drawn to the NHS because of its commitment to patient-centered care and equitable access to healthcare. My clinical background has prepared me to manage diverse cases, and I am eager to contribute to the NHS’s values of compassion and teamwork. Additionally, the opportunities for professional growth, such as engaging in teaching and research, align with my long-term aspirations.”
Background and Motivation Questions Templates
I will start with the important ones and then throw some examples afterwards:
Duty of Candour
Every healthcare professional has a responsibility to be open and honest with patients and their families when something goes wrong during treatment or care.
![[2025] Competency-Based NHS Interview Questions and Answers 8 Chart explaining the Duty of Candour in three steps:
Acknowledge and Inform – Recognize and communicate openly with the patient or their family when something goes wrong.
Apologize Sincerely – Offer a heartfelt apology, showing empathy and taking responsibility.
Take Action and Prevent Recurrence – Provide remedies, explain preventative steps, and engage in learning processes to improve care.](https://scrubtales.co.uk/wp-content/uploads/Duty-of-Candour-Process.png)
This includes situations where the incident has caused, or could potentially cause, harm or distress. This duty involves the following actions:
- Informing the patient, or when appropriate, their advocate, carer, or family, about what has happened.
- Offering a sincere apology to the patient, or their advocate, carer, or family.
- Providing appropriate remedies or support to address the issue and mitigate harm wherever possible.
- Clearly explaining both the immediate and long-term effects of the incident to the patient or their advocate, carer, or family.
Key Responsibilities
It is essential to understand your responsibilities before answering any NHS interview questions. These include:
1. Duty to Patients
- Be transparent and honest with patients or those close to them if an issue arises during their care.
- Offer a genuine apology and explain what steps are being taken to address the situation.
2. Duty to Organisations
- Report adverse incidents, including those that cause harm and near misses, to your organisation.
- Encourage a culture of learning within the organisation by participating in reporting and reviewing processes.
How to Apologise Effectively
When apologising, ensure the following elements are included:
- A clear explanation of what happened.
- Details of any actions being taken to address the harm caused.
- Steps to prevent similar incidents in the future.
Additional Key Points
- Actively participate in regular reviews and audits to monitor and improve team performance. Take proactive steps to resolve any identified issues.
- Familiarize yourself with the clinical governance and risk management processes of the organizations you work for.
- Follow established procedures for reporting adverse incidents and near misses. Early identification of these incidents is crucial for resolving problems, implementing corrective actions, and learning valuable lessons.
SBAR
SBAR is a structured communication tool used in the NHS to convey critical information clearly and efficiently. It stands for:
![[2025] Competency-Based NHS Interview Questions and Answers 9 SBAR Protocol NHS Interview Questions](https://scrubtales.co.uk/wp-content/uploads/SBAR-Protocol-NHS-Interview-Questions.webp)
- Situation: Briefly explain the current issue or concern.
- Background: Provide relevant clinical background or history.
- Assessment: Share your assessment of the situation, including observations or suspected issues.
- Recommendation: Suggest specific actions or next steps required to address the situation.
SBAR technique enhances communication, improves patient safety, and facilitates timely decision-making in clinical settings. This technique should be your ready-to-go NHS interview question, and you should be ready to smash it.
Situation
My name is [Name], and I am a [Position] working on [Ward/Unit Name]. I’m calling about [Patient Name/Identifier] because I’m concerned about their condition. For example, their blood pressure is [low/high], their pulse is [XX], their temperature is [XX], and their Early Warning Score is [XX].
Background
[Patient Name/Identifier] was admitted on [Admission Date] with [Condition, e.g., myocardial infarction or chest infection]. They have undergone [Procedure, e.g., surgery/investigation] during their stay. In the last [XX minutes], their condition has changed significantly. Their latest observations are [XX]. Typically, the patient is [e.g., alert, pain-free, or drowsy].
Assessment
I believe the problem may be [Suspected Issue]. I have already [Actions Taken, e.g., administered oxygen, provided analgesia, or stopped an infusion].
Alternatively:
- I am unsure what the problem is, but the patient is deteriorating.
- I’m not sure what the exact issue is, but I am very concerned about the patient’s condition.
Recommendation
I need you to see the patient within the next [XX minutes]. In the meantime, is there anything specific you’d like me to do, such as stopping fluids or repeating observations?
Difficult Colleague
We all face this NHS interview question, directly or indirectly!
3 Domain Step-wise
- Patient safety
- Support colleague
- Escalate
- If immediate concern, escalate to seniors
- If not, notify seniors/ supervisors
SPIES Protocol
- Seek Information
- Patient Safety
- Initiative
- Escalate
- Support
Question:
“Tell us about a time you had to deal with a difficult colleague and how you managed the situation.”
Answer:
“In my previous role, I encountered a situation where a colleague frequently interrupted during team discussions, which affected the team’s focus and morale.
- Seek Information: I took time to observe the behaviour over several interactions to understand the triggers and their impact on the team. I also spoke privately with other colleagues to gather their perspectives, ensuring I had a complete picture.
- Patient Safety: Although the issue did not directly compromise patient care, I ensured that discussions involving patient decisions remained professional and focused to minimise any risks to patient outcomes.
- Initiative: I decided to address the issue directly and constructively. I scheduled a one-on-one conversation with the colleague in a neutral setting. I used a calm and non-confrontational tone to explain how their behaviour was impacting the team dynamic and sought their input on any underlying concerns.
- Escalate: When the behaviour persisted, I involved my line manager to mediate the situation. Together, we developed strategies to enhance collaboration during meetings.
- Support: I offered to support the colleague in any way they needed, whether it was guidance on team communication or adjusting workflows that might be causing frustration. Over time, they became more mindful of their interactions, and the team dynamic improved significantly.
This experience taught me the importance of addressing conflicts early, maintaining professionalism, and fostering a supportive environment for colleagues.”
Mistake You Did
One of the frequently asked tricky NHS interview questions, where you should be levelled, neither a dangerous mistake to show that you are an unsafe doctor, nor a common mistake which every other candidate is telling.
Be creative and come up with something, I am pretty sure every one of us does something wrong, just safe enough not to seek our indemnity coverage.
Question:
“Tell us about a mistake you made and how you tackled it.”
Answer:
“During a busy shift in the surgical emergency department, I was responsible for assessing new patients referred from A&E. One of the patients I saw complained of upper abdominal pain and nausea. I took her medical history and documented it, noting that she had a history of hyperthyroidism. However, I overlooked her tachycardia, assuming it was related to her thyroid condition, and I didn’t perform a thorough abdominal examination. I diagnosed her with gastritis and moved on to assist with suturing, which I was particularly excited about during that shift.
Later, after returning from the minor OT, I was informed that the patient had been admitted and diagnosed with pancreatitis after a senior colleague reviewed her case and ensured she received prompt care.
Recognising my mistake, I immediately apologised to my seniors for my oversight and acknowledged my error. I also apologised to the patient, as I had been her first point of contact from our team. My consultant was supportive and used this as a learning opportunity, encouraging me to deepen my understanding of pancreatitis and the importance of thorough assessments.
After the shift, I spent time revisiting abdominal examination techniques using online resources, such as Geeky Medics. I made it a habit to perform detailed abdominal examinations for all surgical patients and incorporated sticky notes into my workflow to help prioritise tasks more effectively. This reflection and learning process significantly improved my clinical approach.
For example, shortly afterward, I diagnosed an intestinal perforation in a complex case involving a pelvic stab wound. This thorough assessment earned recognition from my team, reinforcing the importance of reflection and continuous improvement in my practice.”
Here are more competency-based NHS interview questions that you should be aware about:
1. Where do you see yourself in five years?
Answer:
“I aim to specialise in cardiology, contribute to research, and mentor junior doctors, becoming an asset to the NHS.”
2. What inspired you to choose medicine as a career?
I was inspired to pursue a career in medicine after witnessing the dedication of healthcare workers during my childhood. A personal experience with a family member’s illness showed me the profound impact doctors can have on patients’ lives. This motivated me to choose a career that combines scientific knowledge with the opportunity to make a meaningful difference in people’s lives.
3. Why did you decide to pursue your speciality?
I chose internal medicine because it allows me to manage complex cases while focusing on holistic patient care. I enjoy the intellectual challenge of diagnosing multifaceted conditions and coordinating care across specialities. My rotations in internal medicine reinforced my passion for this field and my ability to thrive in dynamic and demanding environments.
4. What challenges have you faced while transitioning to the UK healthcare system?
One significant challenge was adapting to the NHS’s patient-centred and multidisciplinary approach, which differs from the system in my home country. I overcame this by attending NHS induction programs, seeking guidance from colleagues, and familiarizing myself with NICE guidelines. This proactive approach helped me integrate into the system smoothly and provide quality care aligned with NHS standards.
5. Can you share a significant achievement in your career that you’re proud of?
In my previous role, I led an audit aimed at improving the management of diabetic patients in the outpatient department. The audit revealed gaps in monitoring HbA1c levels, and I implemented a streamlined protocol for regular follow-ups. This change improved glycemic control in our patient cohort, which was recognized by the hospital leadership as a best practice model.
6. What makes you an ideal candidate for this position?
My extensive clinical experience, combined with my commitment to teamwork and patient safety, makes me an ideal candidate for this role. I have worked in fast-paced environments where I honed my decision-making and problem-solving skills. Additionally, my familiarity with NHS values and guidelines ensures I can contribute effectively to the trust’s mission.
7. How have your previous roles prepared you for working in the NHS?
My experience in a tertiary care hospital exposed me to a diverse range of medical conditions and interdisciplinary teamwork, similar to the NHS environment. I have managed high patient volumes, conducted audits, and mentored junior colleagues, all of which have prepared me to handle the challenges of working in the NHS.
8. What do you hope to contribute to this NHS trust?
I aim to contribute by bringing my clinical expertise, enthusiasm for teaching, and dedication to patient-centred care. I also hope to support quality improvement initiatives and collaborate with colleagues to enhance patient outcomes, aligning with the trust’s focus on excellence and innovation.
9. What aspects of the NHS culture appeal to you the most?
I deeply admire the NHS’s commitment to providing equitable and accessible healthcare to everyone. The emphasis on teamwork, compassion, and evidence-based practice resonates with my personal and professional values. I’m also drawn to the NHS’s focus on professional development and research opportunities.
10. What do you consider your most significant professional strength?
My strongest attribute is my ability to stay calm and focused under pressure. For example, during a mass casualty event, I successfully triaged patients, prioritised care, and coordinated with the surgical team. This ability ensures I can deliver quality care even in demanding situations.
11. How do you stay updated with advancements in your field?
I regularly read journals such as The BMJ and attend webinars and conferences to stay abreast of advancements. I also participate in CPD activities, including courses on the latest NICE guidelines and clinical updates. This ensures that my practice remains evidence-based and aligned with current best practices and standards.
E. Teaching and Leadership Questions
NHS interview questions often assess your ability to mentor, guide, and lead others in a clinical environment. Leadership and teaching skills are vital in fostering a collaborative team atmosphere and enhancing patient safety.
To prepare effectively, practice answering competency questions with a family member. This can help you improve your confidence and delivery, ensuring your responses demonstrate your skills and experience.
Examples of Teaching and Leadership Questions
| Example Questions | Framework to Use |
|---|---|
| How would you teach a junior doctor about sepsis management? | Simplify, Engage, Instruct |
| Describe a time when you led a team during a challenging situation. | STAR Framework |
| How would you explain the importance of hand hygiene to new staff members? | Practical Demonstration |
| Can you provide an example of when you trained a colleague on a new procedure or protocol? | Structured Teaching Approach |
| How would you handle a situation where team members disagree on a clinical decision? | Mediation Techniques |
| Describe a time when you identified a problem in your department and implemented a solution. | Problem-Solving Framework |
| How would you mentor a colleague struggling to meet their performance goals? | Supportive Coaching Approach |
| What steps would you take to improve patient safety in your department? | Quality Improvement Framework |
| Describe how you would lead a ward round with medical students. | Interactive Leadership Approach |
| How would you manage a team in the event of a significant incident or emergency? | Emergency Leadership Framework |
Tips for Answering Teaching and Leadership Questions
- Use Real-Life Examples: Share specific experiences where you demonstrated leadership or teaching.
- Focus on Outcomes: Highlight how your efforts positively impacted the team or improved patient outcomes.
- Demonstrate Communication Skills: Explain how you effectively communicated complex concepts or motivated your team.
- Highlight Collaboration: Emphasise your ability to work alongside colleagues to achieve shared goals.
Teaching and Leadership Questions Templates
1. How would you teach a junior doctor about sepsis management?
Answer:
“To teach a junior doctor about sepsis management, I would start by simplifying the Sepsis Six framework and explaining its importance. I’d use real-life scenarios to engage them and encourage questions for better understanding. Afterwards, I’d provide them with resources for further learning and arrange a follow-up discussion to reinforce their knowledge.”
2. Describe a time you led a team during a challenging situation.
Answer (STAR Framework):
“S: During a night shift, a patient in cardiac arrest required immediate intervention. T: I was responsible for leading the resuscitation team. A: I assigned tasks—compressions, airway management, and defibrillation—to ensure all roles were covered. I communicated clearly and monitored progress throughout the process. R: The patient was stabilised and transferred to the ICU, demonstrating effective teamwork and leadership.”
F. Clinical Governance Questions
In the NHS interview questions based on clinical governance, the panel assess your understanding of quality improvement, patient safety, and professional accountability. Effective clinical governance not only ensures high standards of care but also benefits the business (NHS trust) by improving patient safety and outcomes, which can enhance the organisation’s reputation and operational efficiency.
These questions often require clear, structured answers that showcase your knowledge and practical experience. When discussing patient experience, it is essential to highlight strategies to improve customer experience, such as managing wait times, setting clear expectations, and proactively addressing concerns. Focusing on these approaches demonstrates your commitment to enhancing customer experience and overall service quality in clinical settings.
Clinical Governance NHS Interview Questions with Answers
1. Tell us about your teaching experience.
I have had the opportunity to teach junior colleagues and medical students during ward rounds and clinical placements. My approach involves simplifying complex concepts, engaging learners through clinical scenarios, and encouraging active participation. For example, I once led a teaching session on sepsis management, using case studies to make the content relatable and interactive. Feedback from attendees highlighted my ability to make topics clear and engaging, which motivates me to continue refining my teaching skills.
2. How do you know that you are a good teacher?
I assess my effectiveness as a teacher through feedback from learners, both formal and informal. For instance, after delivering a teaching session on the management of diabetic ketoacidosis, several junior doctors mentioned they felt more confident handling similar cases. Additionally, I often observe learners applying what they’ve been taught during clinical practice, which reassures me that the teaching was impactful.
![[2025] Competency-Based NHS Interview Questions and Answers 10 Funny meme 6](https://scrubtales.co.uk/wp-content/uploads/Funny-meme-6.webp)
3. What is a Clinical Audit?
A clinical audit is a systematic process of reviewing clinical practices against established standards to ensure that patients receive high-quality care. It involves identifying areas for improvement, implementing changes, and re-auditing to evaluate the effectiveness of those changes. Audits are an integral part of clinical governance, helping to maintain and enhance the quality of healthcare services.
4. Tell us about an interesting audit that you did.
In my previous role, I conducted an audit on the timeliness of antibiotic administration for sepsis patients in the emergency department. The audit revealed delays in administering antibiotics within the recommended one-hour window. Based on the findings, we introduced a sepsis protocol and staff training sessions. A re-audit revealed significant improvement, with over 90% compliance, which had a positive impact on patient outcomes.
5. What are the problems associated with the audit process?
The audit process can face several challenges:
- Data Collection: Accessing accurate and complete data can be time-consuming and sometimes unreliable.
- Engagement: Gaining buy-in from staff to implement recommendations can be difficult, especially in busy settings.
- Sustainability: Changes introduced during an audit may not always be maintained over time.
- Resources: Audits often require time and administrative support, which can be limited in a clinical environment.
6. What is the difference between audit and research?
The main difference lies in their objectives and methodology.
- Audit: Aims to evaluate current practices against established standards to improve patient care. It asks, “Are we doing things right?”
- Research: Seeks to generate new knowledge by answering specific questions or testing hypotheses. It asks, “What is the right thing to do?” Audits focus on quality improvement, whereas research focuses on generating evidence.
7. Tell us about your research experience.
Although I have not yet conducted formal research, I am very interested in pursuing it in the future. I actively engage with academic journals and attend research presentations to understand the methodologies and findings relevant to my field. I am keen to develop research skills and contribute to evidence-based practices as I progress in my career.
8. Do you think all trainees should do research?
Yes, I believe research is an essential component of medical training, as it promotes critical thinking, analytical skills, and evidence-based practice. While not all trainees may directly engage in research, understanding the principles of research and its application in clinical practice is crucial for delivering high-quality patient care.
9. What is evidence-based medicine?
Evidence-based medicine (EBM) is the integration of clinical expertise, the best available evidence from research, and patient preferences to make informed decisions about patient care. EBM ensures that medical practices are up-to-date, effective, and tailored to the individual needs of patients.
10. What is clinical governance? What are the 7 pillars?
Clinical governance is a framework through which healthcare organizations are accountable for continuously improving the quality of their services and safeguarding high standards of care. The 7 pillars of clinical governance are:
- Clinical Effectiveness: Ensuring care is based on the best evidence.
- Risk Management: Identifying and mitigating risks to patients and staff.
- Patient Experience and Involvement: Engaging patients in their care and decision-making.
- Audit: Reviewing practices against standards to improve care.
- Staffing and Staff Management: Supporting staff development and ensuring a competent workforce.
- Education and Training: Maintaining the skills and knowledge of healthcare professionals.
- Information Management: Using accurate data to improve clinical practice.
11. What is DATIX?
DATIX is an incident reporting system used in the NHS to record, track, and manage clinical incidents, near-misses, and complaints.
It enables healthcare organizations to analyze patterns, identify areas for improvement, and implement changes to enhance patient safety and reduce risks.
I recommend having a glance at it, as it was frequently asked in the past as a part of NHS interview questions.
If you want to have a quick look as to how datix looks like, this video is just for you (sarcastically, the number of datix done are usually 20x higher when done by nurses as compared to done by doctors).
5. Freebie Alert: NHS Interview Preparation Checklist
Download your free checklist, which includes:
- Steps to organise your portfolio.
- Common clinical, ethical, and behavioral questions.
- Tips for mastering STAR, SPIES, and CAMP frameworks.
For more advice and resources on NHS interview preparation, check out our expert guidance.
Final Thoughts
The NHS interview is more than a test of your clinical knowledge—it’s an opportunity to showcase your commitment to patient-centred care, your adaptability, and your alignment with NHS values. By preparing thoroughly, mastering key frameworks such as STAR and SPIESABCDE, and practising your responses to clinical, behavioural, and ethical questions, you can approach your interview with confidence and clarity.
Remember, the interview panel wants to see your potential as a compassionate, collaborative, and competent doctor who will thrive in the NHS environment. Every question is an opportunity to showcase your skills, experiences, and motivation to make a difference.
Take the time to prepare, believe in your abilities, and trust the hard work you’ve put into reaching this stage. You’re on the brink of an exciting journey in one of the world’s most respected healthcare systems.
FAQs
How long do NHS interviews usually last?
NHS interviews typically last 30-45 minutes for panel interviews. Station-based interviews may vary depending on the number of stations, with each station lasting around 10-15 minutes.
What should I wear to an NHS interview?
Professional attire is essential. For men, a suit with a tie or smart formal wear is recommended. For women, formal trousers, skirts, or dresses with a blazer are ideal. Ensure your appearance is neat, clean, and professional.
Are NHS interviews conducted in person or online?
Both formats are used. Virtual interviews have become more common since the pandemic, but some trusts may still prefer in-person interviews. Always confirm the format when you’re invited to the interview.
How can I practice for NHS interviews?
You can practice by using mock interviews with colleagues, mentors, or a family member to simulate the interview environment and record your answers to common questions, then review them for clarity and tone, practising frameworks like STAR, SPIES, and ABCDE to ensure structured responses.
What kind of technical preparation is needed for a virtual NHS interview?
For virtual interviews, test your internet connection to ensure it’s stable. Use a quiet, well-lit room with a professional background. Check your camera, microphone, and video conferencing platform beforehand. Dress professionally as you would for an in-person interview.
Can I ask questions during the NHS interview?
Yes, asking thoughtful questions shows your interest in the role and trust. Examples include: “What are the available research opportunities?” “Will I be doing on-calls?” “What opportunities are there for professional development in this trust?” “How does the team foster collaboration and communication?”
How important is it to research the NHS trust before the interview?
Researching the trust is crucial. Understanding their specialities, achievements, and values allows you to tailor your answers and demonstrate your interest in contributing to their mission.
What if I don’t know the answer to a clinical question?
If you’re unsure about a clinical question, respond by acknowledging your uncertainty, but demonstrate your thought process. Mention how you would look up the relevant information or escalate to a senior colleague if necessary. Highlight your commitment to patient safety and teamwork.
Tip: If you are unsure about a clinical question, respond honestly and explain the steps you would take to find the correct answer, such as consulting guidelines or asking a more experienced team member for guidance.
How can I manage interview anxiety?
To manage anxiety: Practice deep breathing or mindfulness exercises. Prepare thoroughly to boost your confidence. Focus on your achievements and remind yourself why you’re qualified for the role. Treat the interview as a conversation rather than a test.
Is it okay to bring notes to the interview?
Yes, it’s acceptable to bring notes or a portfolio with key points about your achievements, but avoid reading directly from them. Use them only as a quick reference if needed.
What happens after the NHS interview?
Post-interview: The panel will score your performance and discuss your fit for the role. Successful candidates are typically contacted within a few days to weeks, depending on the trust. If unsuccessful, you can request feedback to improve for future interviews.