When I first started working in the NHS, many things felt unfamiliar. One day, my consultant asked, “Can you get a red DNAR form, please?”
Like many IMGs, I hadn’t come across DNAR in my home country—but you quickly learn on the job.
In this post, I’ll break down the essentials: What is a DNAR meaning, the red form, the legal status, DNACPR discussion, who signs it, what to fill and how to handle it confidently without getting caught off guard.
What is a DNAR?
DNAR stands for Do Not Attempt Resuscitation.
It's a clinical decision not to perform CPR if a patient’s heart stops or they stop breathing.
Importantly, you need to know that:
- It is not a withdrawal of care.
- It does not mean “do not treat”.
- It only applies to cardiopulmonary resuscitation.
In some hospitals, you might see it called DNACPR or DNR. Because it has red layout, it is sometimes referred to as a Red Form as well.
You’ll better understand the realities of CPR after doing an ALS course for NHS doctors, which covers CPR indications and futility in practice.
DNACPR Form PDF Download
Who Can Discuss and Sign a DNAR?
Who Can Discuss DNACPR
- Consultants or senior registrars should ideally lead DNAR discussions.
- FY2 doctors can initiate discussions, especially if trained, but must inform seniors.
- FY1 doctors may observe or contribute but should not lead without supervision.
- Nurses and ANPs can support conversations but shouldn’t lead decisions unless trained and authorised in specialist settings (e.g. palliative care).
DNAR discussions often involve multiple team members. It helps to be clear on understanding the roles of MDT members when coordinating care decisions.
Who Can Sign a DNAR Form
| Role | Can Sign? | Notes |
|---|---|---|
| Consultant | Yes | Must countersign within 24 hours for DNAR to remain valid |
| Registrar (ST3+) | Yes | Should ideally involve a consultant |
| FY2 Doctor | Yes | Can sign but consultant review mandatory |
| FY1 Doctor | No | Can witness discussions but cannot sign |
| Nurses / HCAs | No | Can initiate conversations but not complete forms |
- Consultants are ultimately responsible for the DNAR decision and should countersign forms.
- Registrars (ST3+) can sign if they are the senior clinician present.
- FY2 doctors may sign a the form in hospitals if no senior is immediately available, but it must be reviewed and countersigned by a consultant within 24 hours.
- FY1 doctors cannot sign the forms under any circumstance.
- Advanced Nurse Practitioners (ANPs) may sign only in community or hospice settings if local policy explicitly allows.
- Nurses/HCAs are not authorised to sign DNAR forms.
Legal Status of DNAR in the UK
- DNAR is a clinical decision, not a legally binding document — but it carries legal responsibilities.
- Doctors are not obliged to offer CPR if it is deemed futile, burdensome, or not in the patient’s best interests.
- If the patient has capacity, they must be involved in the decision.
- The Tracey v Cambridge University Hospitals NHS Trust (2014) case made it clear: Patients have a legal right to be informed about DNAR decisions.
- If informing the patient would cause serious harm, doctors can withhold the discussion — but this must be justified.
- If the patient lacks capacity, you must:
- Complete a Mental Capacity Assessment
- Make a best interest decision
- Consult family or legal proxy
- Family cannot demand or refuse CPR — the final decision rests with the senior clinician.
- DNAR decisions must comply with the Mental Capacity Act 2005 and human rights law.
- Always document the rationale, capacity status, and family discussions in the notes.
- DNAR forms should be reviewed regularly, especially on discharge, readmission, or condition change.
It’s essential to follow proper legal protocols for DNAR to protect both the patient and yourself. Make sure your medical indemnity insurance for NHS doctors covers end-of-life care documentation.
Common IMG Doctor Challenges (and Solutions)
| Challenge | Solution |
|---|---|
| Asked to “get red form” with no idea what that is | It’s the DNAR form – ask senior or check ward folder |
| Don’t know how to fill it | Use this guide, ask registrar/consultant to supervise once |
| Confused about capacity | Read MCA basics – capacity = understand, retain, weigh, communicate |
| Don’t know where to check for existing DNACPR | EPR → Alerts → Scanned docs → Discharge summaries |
| Unclear when to initiate discussion | Chronic illness + frailty = always consider on admission |
| Form returned because consultant didn’t sign in 24h | Message consultant directly or leave form with sticky note reminder |
When to Discuss DNAR
This is one of the difficult questions to answer, but recommendations include:
Best time:
- On admission for patients with chronic illness or frailty.
- Before elective procedures or major surgery in high-risk patients.
- When the patient deteriorates unexpectedly.
- During discharge planning if resuscitation would not be appropriate.
Avoid:
- Waiting until crisis moments.
- Rushed decisions in resus bays or during on calls.
DNAR and Capacity
If the patient has capacity, you have to involve them in the decision.

If they lack capacity, then:
- You must complete a Mental Capacity Assessment (MCA).
- Consult family or legal proxy (best interest decision).
- Document all discussions clearly.
- Add “Patient lacks capacity – discussed with NOK” on the DNACPR form.
Remember, ff the patient appears confused, a proper confusion screen and delirium tools assessment should be done before determining capacity.
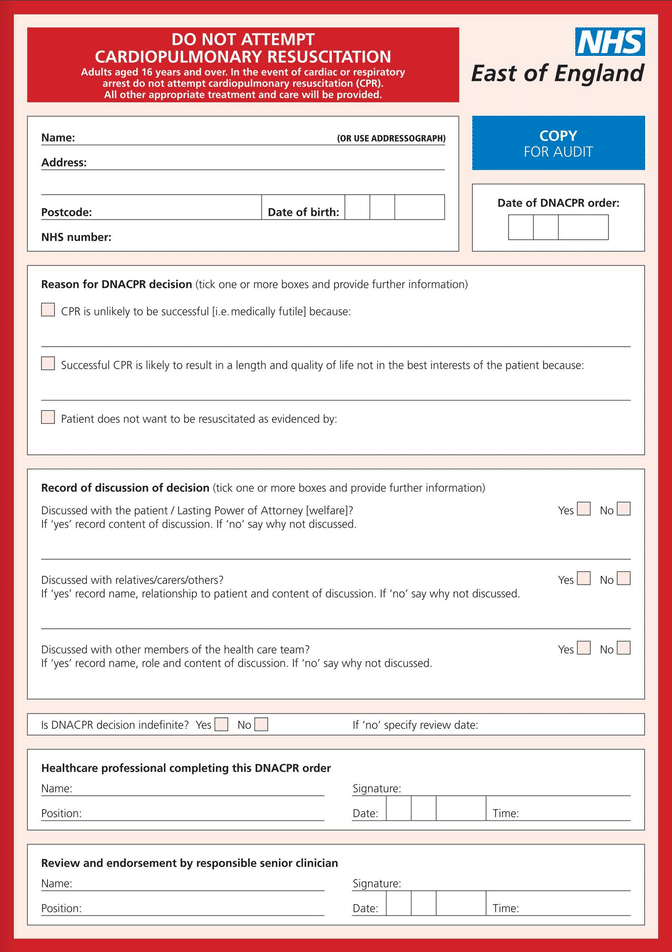
What’s the DNAR “Red Form” Everyone Talks About?
The red form is a two-page document used in most NHS trusts. It’s bright red so it’s easily visible in notes.
- One copy stays in the hospital file.
- The original goes with the patient (to nursing homes, home, or hospice).
Always complete two copies, depending on your Trust’s policy.
Where to Find the DNAR Form
Here’s where it usually hides:
- Hospital Intranet: Search “DNAR” or “Resuscitation Form”.
- Paper stores: Many wards have them printed and ready.
- ED / MAU / Resus Room: Always stocked.
- Ask the ward clerk or nurse in charge—they usually know.
How to Check Existing DNAR Status
You don’t always need to start from scratch.
Before writing a new DNAR form, check if one already exists:
| Where to Check | What You Might Find |
|---|---|
| Discharge summaries | Previous DNACPR status in “Treatment Plan” section |
| EPR / Electronic patient records | Scanned forms, alerts, prior discussions |
| Alert banners | Red DNAR tag in system like Cerner / EPR |
| GP letters or nursing home papers | May mention prior DNACPR |
| Family/carers | Can often tell you if one exists |
Previous DNAR Form Exists
If the patient had the form previously, or one exists already, it is important to validate the continuity.
Whenever a patient is admitted who had a DNACPR form previously, you have to ask there wishes:
You had a DNAR previously, are you happy to continue with the same?
It is important to document the conversation and make sure they understand it fully. If they lack capacity, you have to confirm with the family or NOK (next of kin) or legal proxy.
DNAR Validity: Key Points
- Valid for in-hospital stay unless marked for community.
- Consultant must sign within 24 hours.
- DNACPR forms must be reviewed periodically, especially on readmission or change in condition.
- If patient is discharged, a copy goes with them.
How to Fill DNAR Form: Step-by-Step
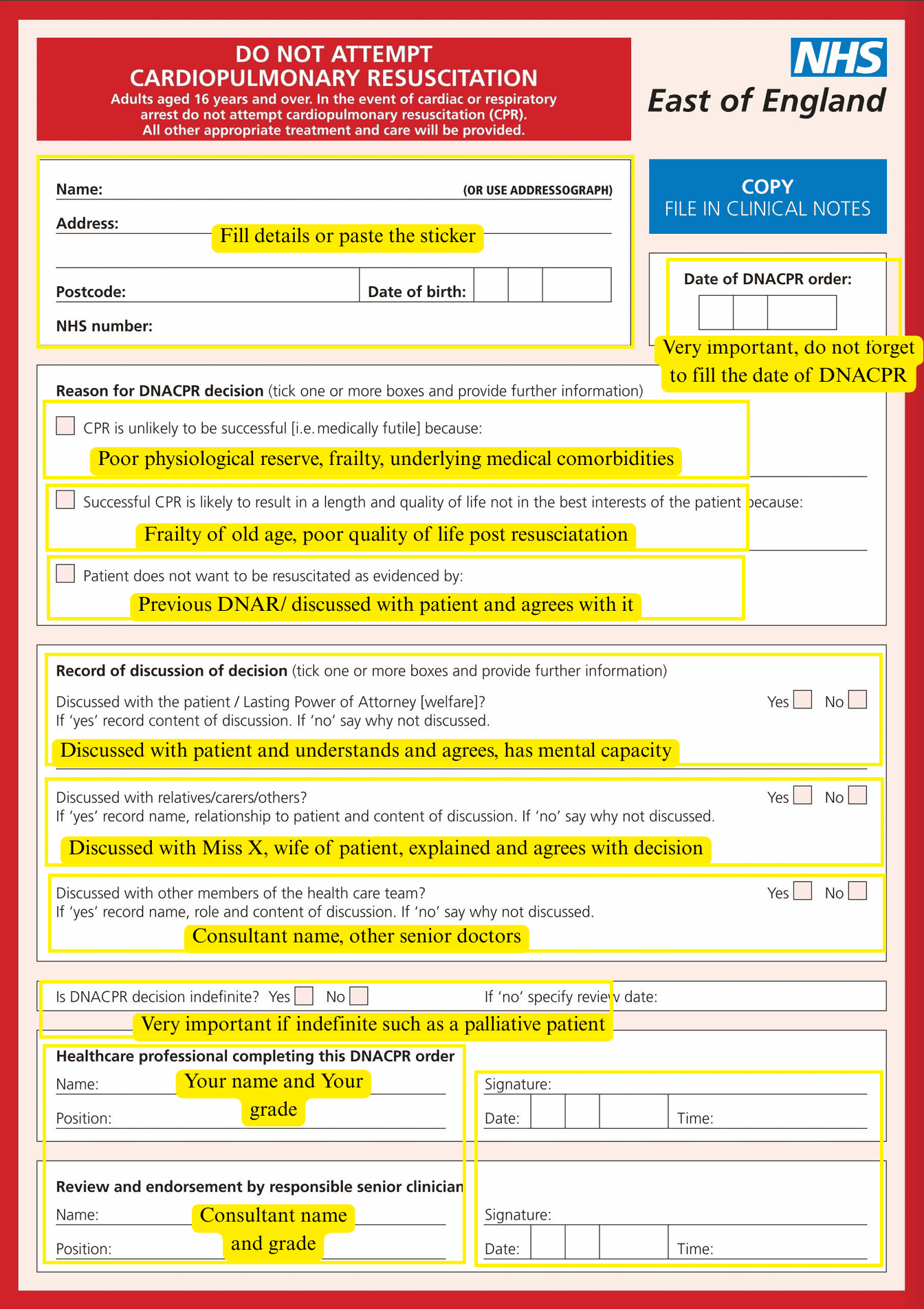
How to Fill DNACPR Form
Patient details
Fill details or paste the sticker: Name, hospital number, date of birth, NHS number, etc.
Reason for DNACPR
Document the reasoning for completing DNAR form, if previous form exists, mention the same.
Record of Discussion of decision
If patient has capacity, document discussed with patient.
If patient lacks capacity, document discussed with NOK (next of kin), or legal guardian or person holding LPA (Lasting Power of Attorney)
Document the senior you discussed with, usually the consultant signing the form.
Is DNACPR indefinite?
Mostly DNACPR is indefinite, however, where reversible causes are identified and a clinical decision is made to reverse the DNACPR, this should not be ticked. However, this decision lies on the consultant.
For example, an elderly patient aged 98 with significant underlying comorbidities and frailty, indefinite sounds right.
Signatures and Grades
Do not forget to get the form signed by consultant as it is legally valid only if signed by consultant. This should be done within 24hrs of completing the form.
Date of DNACPR
Do not forget to mention this part as it crucial for documentation and future references.
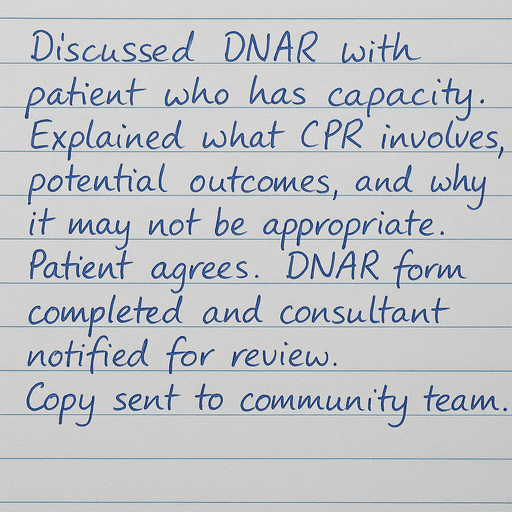
Documentation in Notes
Don’t just fill the form — document the full discussion in medical notes.
Use this format:
“Discussed DNACPR with patient who has capacity. Explained what CPR involves, potential outcomes, and why it may not be appropriate. Patient agrees. DNACPR form completed and consultant notified for review. Copy sent to community team.”
Or:
“Patient lacks capacity. Completed MCA form. DNACPR discussed with family/NOK in best interest. DNACPR form completed. Consultant to review.”
Accuracy in writing DNAR forms is just as important as filling professional documentation like the CREST form for MSRA and training.
What to Discuss in a DNAR Conversation
In a nutshell, here’s what you should cover:
- What CPR is (and what it isn’t).
- Success rates and risks (e.g., broken ribs, poor outcomes in frailty).
- That other care continues regardless (fluids, antibiotics, oxygen).
- Patient wishes and values.
- Family views (if the patient lacks capacity).
- Most importantly, highlight this is a medical decision and the medical team can make the decision even if the family or the patient is not in agreement given the decision is in best interest of the patient.
Explanation of CPR (Cardiopulmonary Resuscitation)
- Define CPR: Explain that CPR is an emergency procedure to try to restart a person’s heart or breathing if it stops.
- Describe the process: It involves forceful chest compressions, electric shocks to the heart (defibrillation), artificial ventilation, and emergency medications.
- Purpose of CPR: Emphasize that CPR aims to restore circulation and breathing, but its effectiveness depends on the person’s overall health.
Risks and Likelihood of CPR Success
- Low success rate: Highlight that CPR has a low success rate, especially in very sick or frail patients (only about 1–2 in 10 patients have their heart/breathing restarted).
- Possible injuries: Explain that CPR is invasive and can cause physical trauma – for example, it often leads to broken ribs, lung injuries, or other organ damage from the force of compressions.
- Poor outcomes: Even if CPR does restart the heart, the person may not fully recover – many who survive CPR remain very unwell or never regain their previous level of health.
- Context of illness: Make it clear that in the context of advanced illness or end-of-life, CPR is likely to be futile or only briefly prolong life, which is why a DNAR is being considered.
Alternatives to CPR (Focus on Comfort)
- Allow natural death: Discuss the approach of allowing a natural, peaceful death when the time comes, rather than attempting aggressive resuscitation that could cause suffering.
- Comfort-focused care: Emphasize that if the patient’s heart stops, the team will prioritize keeping them comfortable – for example, providing pain relief, oxygen, and calming measures instead of CPR.
- Dignity and support: Reinforce that the goal is to ensure the patient’s dignity and relieve distress at end of life, rather than performing interventions that are unlikely to help.
- Treat reversible issues: Clarify that any treatable, reversible problems will still be addressed promptly. (For instance, if a specific reversible complication arises, doctors would still provide appropriate intervention despite a DNAR order.)
Clarify What DNAR Means
- Meaning of DNAR: State that DNAR stands for “Do Not Attempt Resuscitation” – this means that if the patient’s heart or breathing stops, the medical team will not perform CPR in that event.
- Scope is limited to CPR: Emphasize that DNACPR applies only to CPR. It does not apply to other treatments or interventions – the patient will continue to receive all other appropriate medical care.
- Advance care planning: Explain that having a DNAR order is a standard part of advance care planning. It is done to respect the patient’s wishes and well-being, and does not imply giving up on the patient’s care.
- Documentation: Mention that the decision will be recorded on a special form in the patient’s medical records so all healthcare professionals are aware of it in an emergency.
Clarify What DNAR Does Not Mean
- Not “do not treat”: Reassure that DNAR does NOT mean no other care will be given. The patient will still receive full medical treatment for any conditions (medicines, oxygen, surgery, etc.) up until the very end – it only excludes the act of CPR.
- Not abandoning the patient: Make clear that DNAR does not mean the healthcare team is abandoning the patient or “letting them die” without care. All supportive care will continue; the team remains fully committed to the patient’s comfort and treatment.
- Not euthanasia or hastening death: Emphasize that a DNACPR order does not cause death or speed up dying – it simply means if a natural death occurs, the team will not try to restart the heart with CPR. The focus is on allowing a natural passing without undue trauma.
- Address “giving up” fears: If the patient or family expresses worry that a DNAR feels like “giving up,” firmly reassure them that this is not the case – the healthcare team will still actively care for the patient in every other way.
Reassure That Other Treatments Will Continue
- Ongoing care: Emphasize that aside from CPR, nothing else is being withheld. All other appropriate treatments – for example, antibiotics for infections, fluids, oxygen, surgery or procedures for treatable issues – will continue as needed.
- Symptom management: Reiterate that the medical team will provide aggressive symptom control and comfort measures (pain relief, breathlessness management, nursing care) to maintain the patient’s comfort and dignity.
- Unchanged commitment: Make it clear that the patient’s overall care plan remains the same in terms of effort and attention. The DNAR decision simply prevents causing additional harm from CPR, but does not change the commitment to the patient’s well-being.
- Review if situation changes: Mention that DNACPR decisions can be revisited. If the patient’s condition or wishes change, the care team can review and update the plan (the DNAR is not “set in stone” if circumstances were to improve unexpectedly).
Legal and Capacity Considerations
- Patient capacity and choice: If the patient has mental capacity, involve them directly in the DNAR discussion. Patients have the right to make decisions about CPR – for instance, a patient may choose to refuse CPR and can formalize that refusal in an Advance Decision to Refuse Treatment (ADRT) document.
- No patient consent needed for DNAR: Explain sensitively (especially to family) that DNAR is ultimately a medical decision. Doctors do not require formal consent to write a DNACPR order if CPR would be futile, but good practice (and legal guidance) is to consult with and inform the patient or family beforehand.
- Best interests if no capacity: If the patient lacks capacity (e.g. due to dementia or unconsciousness), the healthcare team will make a best-interest decision about CPR. They will consider any prior wishes (advance directives) and involve the family or next of kin in the discussion for insight, following the UK Mental Capacity Act principles.
- Doctors’ obligations: Make it clear that doctors will not offer or perform CPR if they believe it will not work or would only cause more suffering. Doctors are not obligated to give treatments that have no benefit, even if family members request it. The medical team’s duty is to recommend what is in the patient’s best interest.
- Legal framework: Reassure that the DNAR decision is made according to national guidelines and law. For example, a Court of Appeal case (Tracey, 2014) established that patients (or their families) must be informed about a DNACPR decision unless informing them would cause serious harm. All discussions and decisions will be documented clearly in the patient’s notes for transparency and future reference.
Addressing Patient and Family Concerns
- Encourage dialogue: Invite the patient and family to share their thoughts, questions, and fears throughout the conversation. Listen actively to their concerns and acknowledge their emotions (such as anxiety, sadness, or confusion).
- Clarify misconceptions: Gently correct any misunderstandings about DNAR. For example, if they fear the team is “giving up on the patient,” address this by explaining the continued care and the compassionate reasoning behind avoiding CPR.
- Empathy and reassurance: Use empathetic language and reassure them that the primary goal is the patient’s comfort and dignity. Emphasize that the healthcare team wants to spare the patient unnecessary suffering, and that this decision is made with the patient’s best interests at heart.
- Check understanding: Throughout the talk, check that the patient/family understand what is being explained. You can ask them to repeat key points or ask if they have any questions, to ensure clarity. Encourage them to take their time and offer to revisit any aspect of the discussion.
- Handling disagreement: If the patient or family is upset or disagrees with the DNAR decision, remain calm and provide a further explanation of the medical reasoning. Acknowledge their feelings. If they continue to strongly object, propose involving a senior doctor or getting a second opinion for further reassurance. This shows respect for their concerns and ensures that every avenue is explored in the patient’s best interest.
Final Tips for Junior Doctors
- Never fear the DNAR form — it’s a communication tool, not a legal minefield.
- When in doubt, ask your registrar or consultant.
- Always document discussions thoroughly.
- Respect the patient’s dignity, autonomy, and best interests.
Want to showcase your communication and documentation skills? Mention DNAR discussions in your TRAC supporting statements for IMG doctors.
Takeaway Summary
| What? | Why It Matters |
|---|---|
| DNAR = No CPR | Not a withdrawal of treatment |
| FY2 can sign | Consultant must review within 24h |
| Discuss early | Especially in frailty, chronic disease |
| Capacity matters | MCA and best interest discussions are essential |
| Form = 2 pages | One copy + one original for patient/community |
| Check before writing new | EPR, alerts, previous summaries often hold clues |
FAQs
Can DNAR be overridden in an emergency?
Yes, if clearly inappropriate (e.g., form outdated, not found), CPR may be started until clarified.
Does DNAR mean no ICU or intubation?
Not necessarily. DNACPR refers only to CPR. Other escalation levels (e.g., NIV, HDU) are separate discussions.
Can family refuse DNAR decision?
No. If the patient lacks capacity, family views are considered—but final call lies with clinical judgment.
Can patients request DNACPR themselves?
Yes, if they have capacity. You should respect and document their wishes.
Where can I get a blank DNAR form?
Check your hospital’s intranet or ask the resus team/ward clerk.
Can I do DNACPR discussions during on-calls?
Yes, but avoid rushed conversations unless urgently needed.