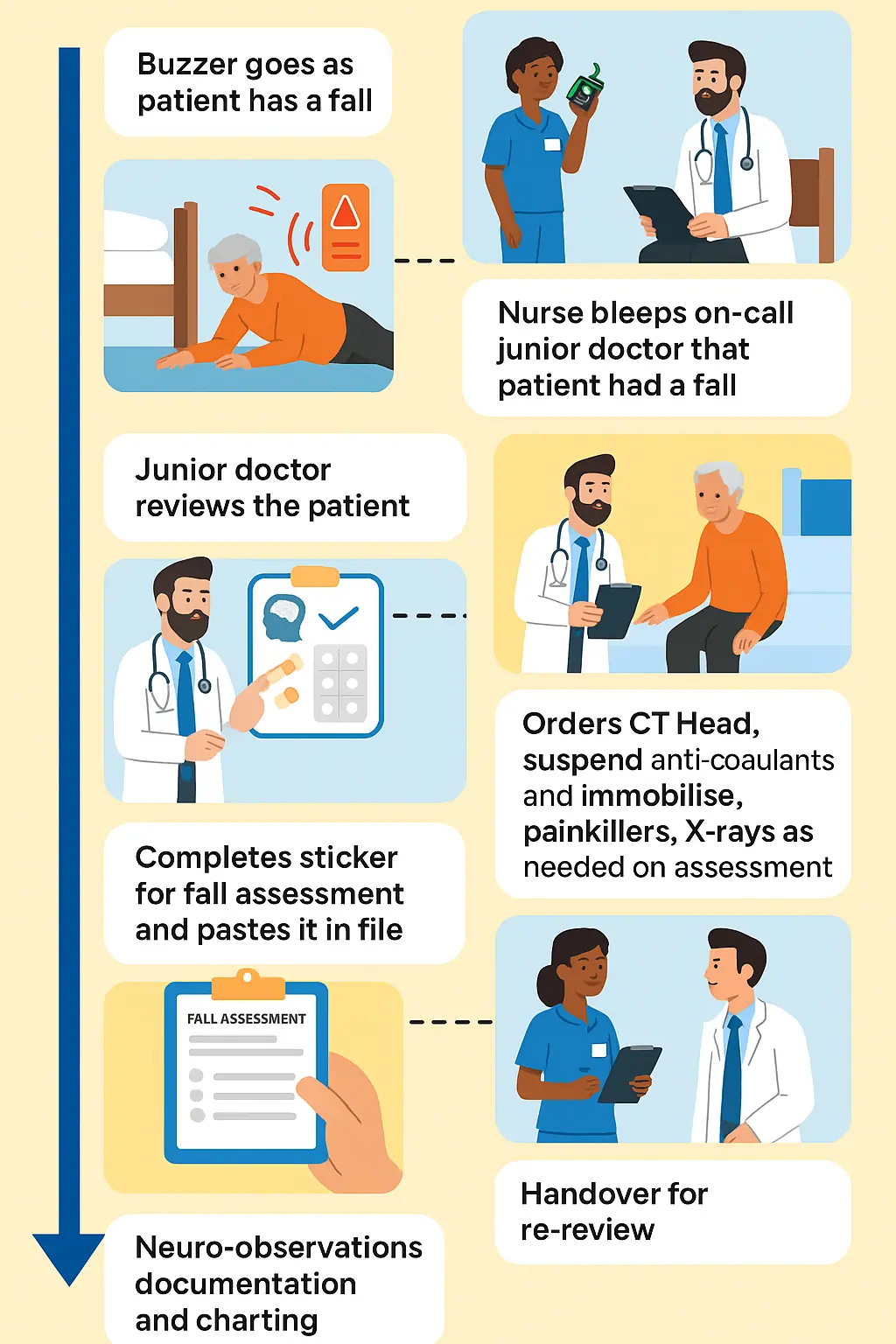
You’re halfway through an on-call shift when a buzzer goes off.
Moments later, the nurse bleeps: “Doctor, patient in bed 5 has fallen.”
Yes, we’ve all been there.
As a junior doctor, knowing how to confidently and safely manage a post-falls assessment is essential. This isn’t just a tick-box exercise – it’s a critical process that helps you spot injuries, rule out life-threatening causes, and prevent further harm.
In this post, we’ll walk through the whole step-by-step post-fall approach tailored for NHS ward settings – including safety checks, history taking, examination, imaging, medication review, escalation, and documentation.
Post-Falls Assessment Checklist
- Ensure scene safety before approaching the patient.
- Do not mobilise until serious injury is excluded.
- Check for DNACPR status.
- Look for red flags: head injury, suspected fractures (shortened/externally rotated leg, spinal tenderness).
- Before fall: symptoms? (dizziness, chest pain, palpitations, blackout).
- Past falls and relevant medical history/medications.
- During fall: witnessed/unwitnessed, head strike, loss of consciousness.
- After a fall: confusion, pain, and mobility.
- Airway: patent?
- Breathing: rate, O₂ sats.
- Circulation: HR, BP (postural if safe), cap refill.
- Disability: GCS, pupils, limb movement.
- Exposure: injuries, bleeding, skin changes.
- Full set of observations.
- Escalate if NEWS2 triggers.
- Capillary blood glucose.
- Head/Face: lacerations, swelling, scalp tenderness.
- C-Spine: midline tenderness, deformity – immobilise if suspected.
- Spine: palpate thoracic/lumbar spine.
- Hips: look, palpate, heel strike, log roll.
- Limbs: swelling, deformity, tenderness.
- Neuro: cranial nerves, power, sensation.
- Gait: only if safe.
- Oral analgesia if mild.
- Reassess after moving or imaging.
- IV opioids ± antiemetic if severe.
- CT Head: if head injury per NICE.
- X-Rays: pain, deformity, inability to mobilise.
- ECG: rule out arrhythmia.
- Bloods: FBC, U&Es, CK, glucose, coagulation.
- Optional: lying/standing BP, ECHO if needed.
- Anticoagulants/antiplatelets – stop/adjust if bleeding.
- Hypoglycaemia-inducing drugs – insulin/OHA.
- FRIDs – sedatives, opioids, antipsychotics.
- Antihypertensives – review if hypotensive/postural drop.
- Complete post-falls sticker/form.
- Document escalation plan and pending results.
- Record history, exam, obs, red flags, actions.
- Communicate injuries found, pending investigations, and re-review needs.
- Highlight high-risk patients needing enhanced monitoring.
Documentation
Why Post-Falls Assessment Matters
Falls are one of the most common inpatient incidents and are a major patient safety concern.
In elderly patients, they’re often a marker of frailty, and they carry serious risks:
- Head injuries (especially if anticoagulated) – even minor trauma can cause subdural bleeds.
- Hip fractures are associated with high morbidity and mortality.
- Spinal injuries, especially in patients with osteoporosis or after a fall from standing height.
- Long lie complications – rhabdomyolysis, acute kidney injury, hypothermia, and pressure sores.
NICE guidelines emphasise that every inpatient fall should trigger a rapid, structured review. This is crucial as it helps in identifying critical injuries and helps establish a safe plan before a full falls risk assessment can be completed.
NICE & Local Policy Reminders
Junior doctors must get acquainted with their local trust guidelines as well as NICE guidelines for falls assessment.
In a nutshell, the following are the general key points you must know:
- Falls assessment must be completed within 6 hours of admission or the incident.
- If delayed (e.g. life-saving surgery or resuscitation), clearly document why.
- Immediate risks – such as a confused patient trying to mobilise unsafely – should be addressed right away. Don’t wait for the paperwork.
- Falls care plans are mandatory for:
- Patients aged 65+
- Patients aged 50–64 with medical conditions that increase fall risk (e.g. Parkinson’s, advanced arthritis, neuropathy).
Falls Care Plan – Who Needs One?
All patients aged 65 or older
Patients aged 50–64 with conditions increasing fall risk, such as:
- Parkinson’s disease
- Stroke or TIA history
- Dementia or cognitive impairment
- Severe arthritis
- Peripheral neuropathy
- Visual impairment
First Things First: Stop and Check
Your first job during the post-falls assessment is to ensure safety and prevent further harm:
- Do NOT move the patient until you’ve excluded serious injury. This means resisting the instinct to “help them up” until you’ve done a quick assessment.
- Look for obvious signs of fracture: shortened and externally rotated leg, severe hip or groin pain, inability to weight-bear.
- If you suspect a spinal injury – neck pain, midline cervical spine tenderness, altered sensation – keep the patient flat, support the head and neck, and call for senior help.
Before doing anything else, check their DNACPR status so you’re prepared if they deteriorate suddenly.
Quick History at the Scene
Once they are safe and stable enough to talk:
- Before the fall: What were they doing? Did they feel dizzy, lightheaded, or have chest pain? Were they trying to rush to the toilet?
- During the fall: Was it witnessed? Did they trip on something (mechanical fall) or lose consciousness? Did they hit their head or back?
- After the fall: Were they able to get up? Any confusion, headache, or new pain?
- Previous falls: How many in the last year? Were any injuries sustained?
- Relevant medical history & meds: Cardiac disease, Parkinson’s, neuropathy, sedatives, antihypertensives, anticoagulants, insulin.
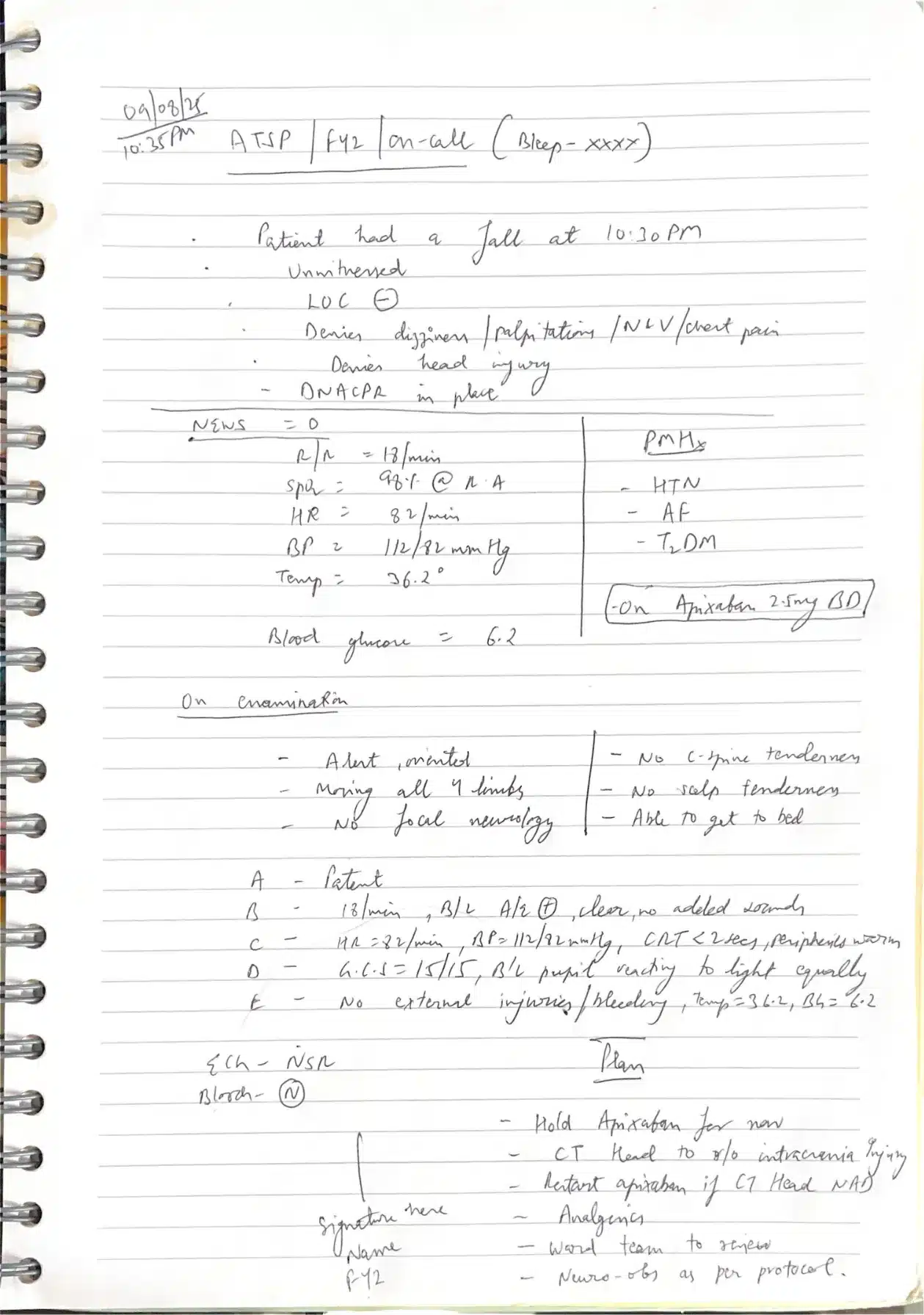
The typical points we record in the notes include:
- Witnessed? Unwitnessed?
- LOC present (loss of consciousness)
- Head injury?
- Neurological deficits?
Even a brief history during post-falls assessment here can guide your injury search and reveal possible causes, such as postural hypotension, hypoglycaemia, or arrhythmia.
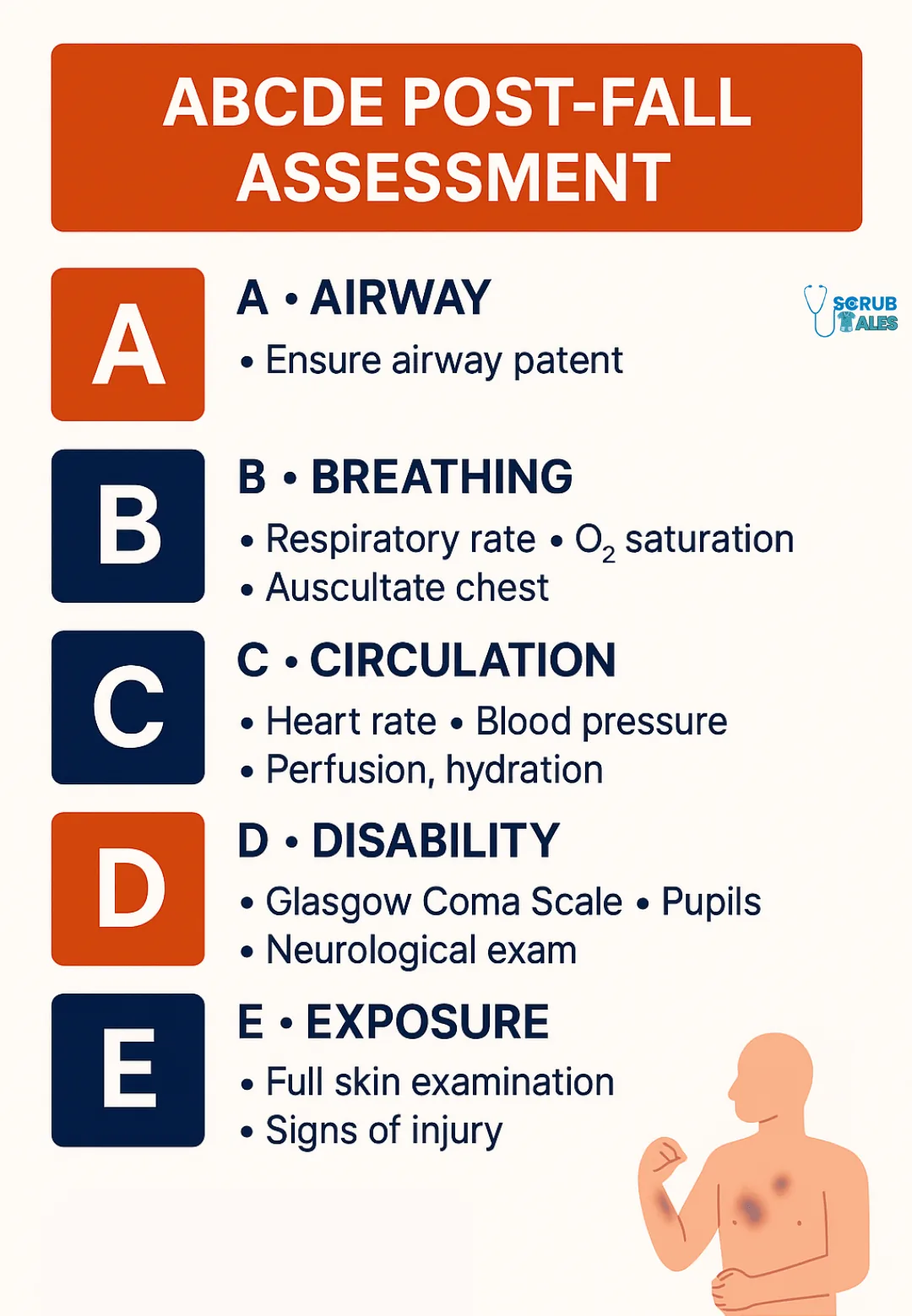
Initial Observations: NEWS2 + ABCDE
Think of an acutely unwell patient and assess the patient using the ABCDE approach:
- Airway – patent? Risk of obstruction from vomit or facial injury?
- Breathing – RR, oxygen saturations, work of breathing.
- Circulation – HR, BP (consider postural if safe), capillary refill.
- Disability – GCS, AVPU, pupils, limb strength.
- Exposure – Check for bleeding, lacerations, bruising, swelling.
Do a full NEWS2 and finger-prick glucose.
It is essential to identify early if the patient is unstable, as this can help in early escalation and review by a senior and possibly the acute care team once you have completed the falls assessment.
Focused Head-to-Toe Examination
Once stable, examine systematically:
- Head & face: Lacerations, swelling, scalp tenderness, boggy haematoma.
- C-spine: Midline tenderness, step deformity, reduced neck movement. Immobilise if any suspicion.
- Spine: Palpate thoracic/lumbar spine for tenderness, deformity, or step-offs.
- Hips:
- Look: Limb shortening, external rotation.
- Palpate: Groin/hip tenderness.
- Heel strike test: Gentle tap to heel – pain suggests fracture.
- Log roll: Pain on minimal movement may indicate a fracture.
- Limbs: Check joints above and below any pain site for swelling, deformity, or restricted range.
- Neuro: Cranial nerves, limb power, sensation, coordination.
- Gait: Only assess if safe. Never force mobilisation.
Tip: In frail patients, injuries may be subtle. A “minor” fall can still cause significant harm and should be excluded during post-falls assessment.
Pain Relief (Don’t Forget This!)
- Offer oral analgesia early for minor pain.
- For significant pain or when awaiting imaging, consider IV opiates with antiemetic cover.
- Always reassess pain, especially after moving the patient or following imaging.
Pain control not only improves comfort but also allows better cooperation with examination and investigations while completing post-falls assessment.
Investigations – What to Order
Base your choices on the history and exam:
Always Consider:
| Test | Why it matters |
|---|---|
| CT Head | Head injury, anticoagulated, confused, fall from height – follow NICE criteria |
| X-rays | Pain, deformity, or inability to mobilise |
| ECG | Identify arrhythmia, conduction abnormality |
| Bloods | FBC, U&Es, CK (if long lie), glucose, coagulation, ABG if necessary |
Optional:
- Lying & standing BP – assess for postural hypotension (usually done by ward day team)
- ECHO and 24-hour TAPE– if cardiac cause suspected (usually outpatient)
It is important to hand over to the next on-call team for any scans or X-rays you investigate. This marks the completion of your post-falls assessment duties.
If bleeding suspected, temporarily stop anticoagulants and escalate to senior for risk–benefit discussion.
Review Medications
Falls are a good opportunity for a quick medication safety check:
- Anticoagulants/antiplatelets – Stop or adjust if bleeding risk; consider reversal if appropriate. Remember to use anti-embolism stockings for VTE prophylaxis to ensure medico-legal safety.
- Fall risk increasing drugs (FRIDs) – Sedatives, hypnotics, opioids, antipsychotics, tricyclic antidepressants.
- Antihypertensives – If hypotensive or with postural drop, review timing/dose.
- Insulin / Oral Hypoglycaemics – If hypoglycaemia contributed, adjust regimen.
- Polypharmacy – Liaise with pharmacist; consider deprescribing in frailty.
Documenting Post-Falls Assessment
Clear records are vital for continuity and governance:
- Use the post-falls assessment sticker or form.
- Document history, exam, observations, red flags.
- Record what actions you took (analgesia, imaging, escalation).
- Handover pending results and re-review needs.
Important: If you suspect head injury, do not forget to request neuro-obs (neurological observations) for the patient.
Escalation & Safety Planning
Some patients will need extra measures after a fall:
- 1:1 nursing for confused/wandering patients.
- Bed near the nurses’ station or motion alarms.
- MDT referrals – physio for mobility, OT for safety assessment, geriatrics for comprehensive review.
- Document any special measures and ensure nursing staff are aware. Ensure nurses bleep if there are any changes in the patient’s status, such as focal neurology deficit.
Conclusion: What to Take Away
Being beeped to a fall isn’t just another job – it’s an opportunity to protect a vulnerable patient. Doing ALS often helps junior doctors tackle difficult situations during on-call shifts and is usually mandatory before you start.
A calm, structured post-falls assessment will help you:
- Identify and treat injuries early
- Prevent deterioration
- Communicate and document effectively
- Put measures in place to prevent future falls
- Falls happen – but with the right approach, you can reduce the harm they cause.
Here is a cheatsheet for post-falls assessment in case you need to save it: