Medicine often feels like detective work. Sometimes, a patient presents with a picture-perfect history, the kind that jumps straight out of a textbook. The diagnosis seems obvious, and the path ahead looks straightforward. But just when you think you’ve solved the puzzle, the pieces don’t fit.
This is one of those cases.
A young woman walked into our emergency department, exhausted from travel and struggling to walk. Every detail of her story pointed towards Guillain-Barré Syndrome (GBS), a rare but serious autoimmune condition that can paralyse patients within days. In fact, it was such a “classic” presentation that the entire team moved quickly — GBS is an emergency, and missing it could cost a life.
But as the hours passed, subtle inconsistencies began to appear. Reflexes that were absent one moment returned the next. Weaknesses that seemed severe faded when she wasn’t being observed. Investigations — blood work, scans, nerve studies — told a different story from the one we expected.
What started as a race against time to prevent respiratory failure soon turned into a lesson in listening beyond the obvious — to the patient, to her family, and to the hidden layers of her life.
As William Osler once said:
“A good physician treats the disease. A great physician treats the patient who has the disease.”
This is the story of how a textbook diagnosis transformed into a journey through neurology, psychiatry, and the human mind. Cases like this remind us how reflection and structured evaluation often form the basis for meaningful clinical audits.
Presenting Complaint
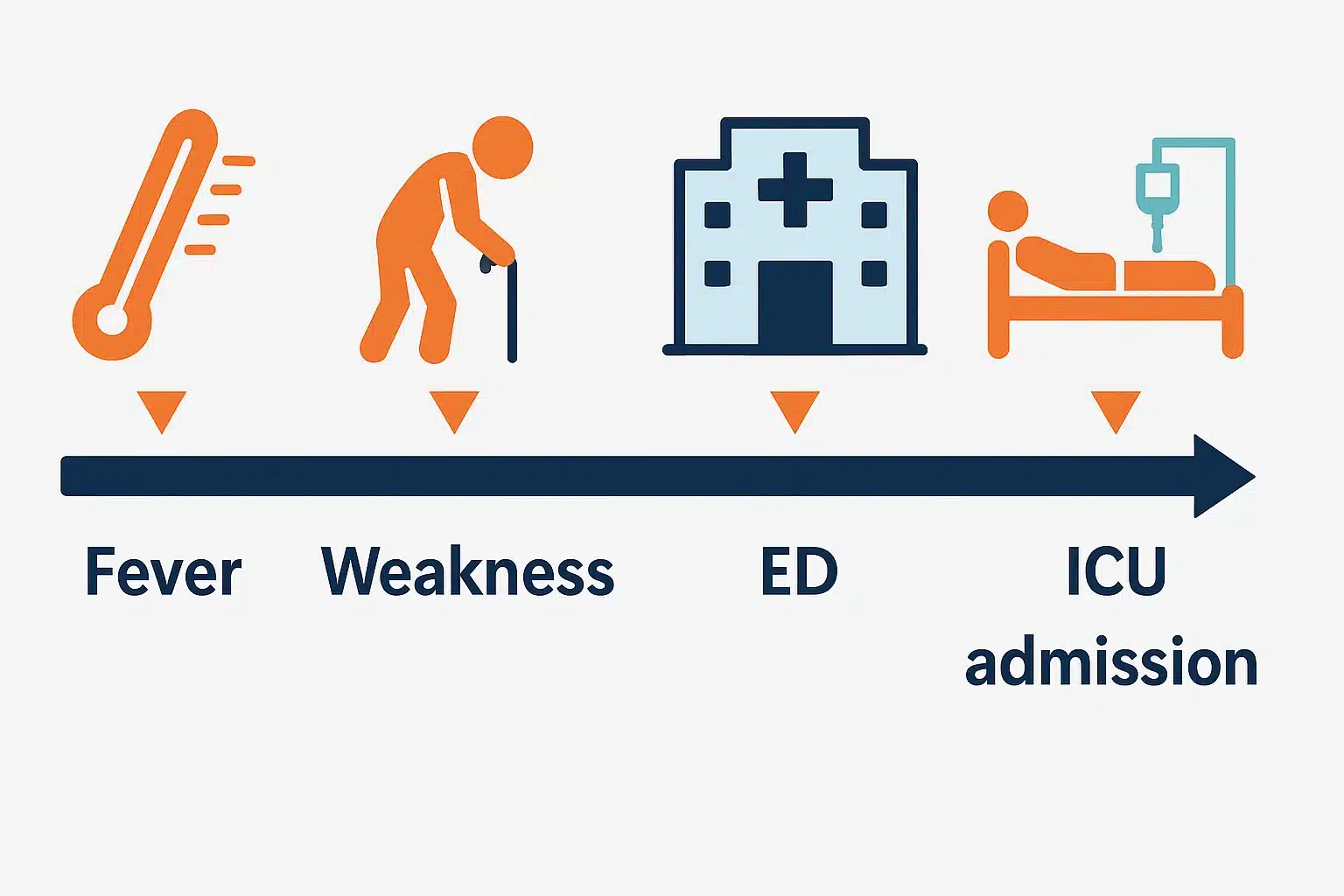
A 37-year-old female arrived at our Emergency Department at around 6:30 pm, straight from the airport. She was accompanied by her sister and one-year-old child.
- Progressive weakness in both legs, lasting for about a week
- She had already seen multiple doctors abroad
- Prior investigations were reportedly insignificant
- Fever and gastroenteritis about two weeks earlier
- Weakness developed gradually after this illness
The story was almost textbook:
- Bilateral foot weakness
- Recent infectious trigger (fever + gastroenteritis)
- Diminished reflexes on initial examination
All of this pointed strongly towards Guillain-Barré Syndrome (GBS) — a frightening autoimmune condition that can progress rapidly to paralysis and even respiratory failure.
This was considered a medical emergency. Treatment needed to be started quickly to prevent potentially life-threatening complications.
Just like recognising acute acidosis or alkalosis in an emergency, spotting early signs of GBS is all about quick pattern recognition
Consultant’s Insight
Our senior consultant neurologist was called immediately to examine the patient. His approach was meticulous, starting with a detailed history and then a physical examination.
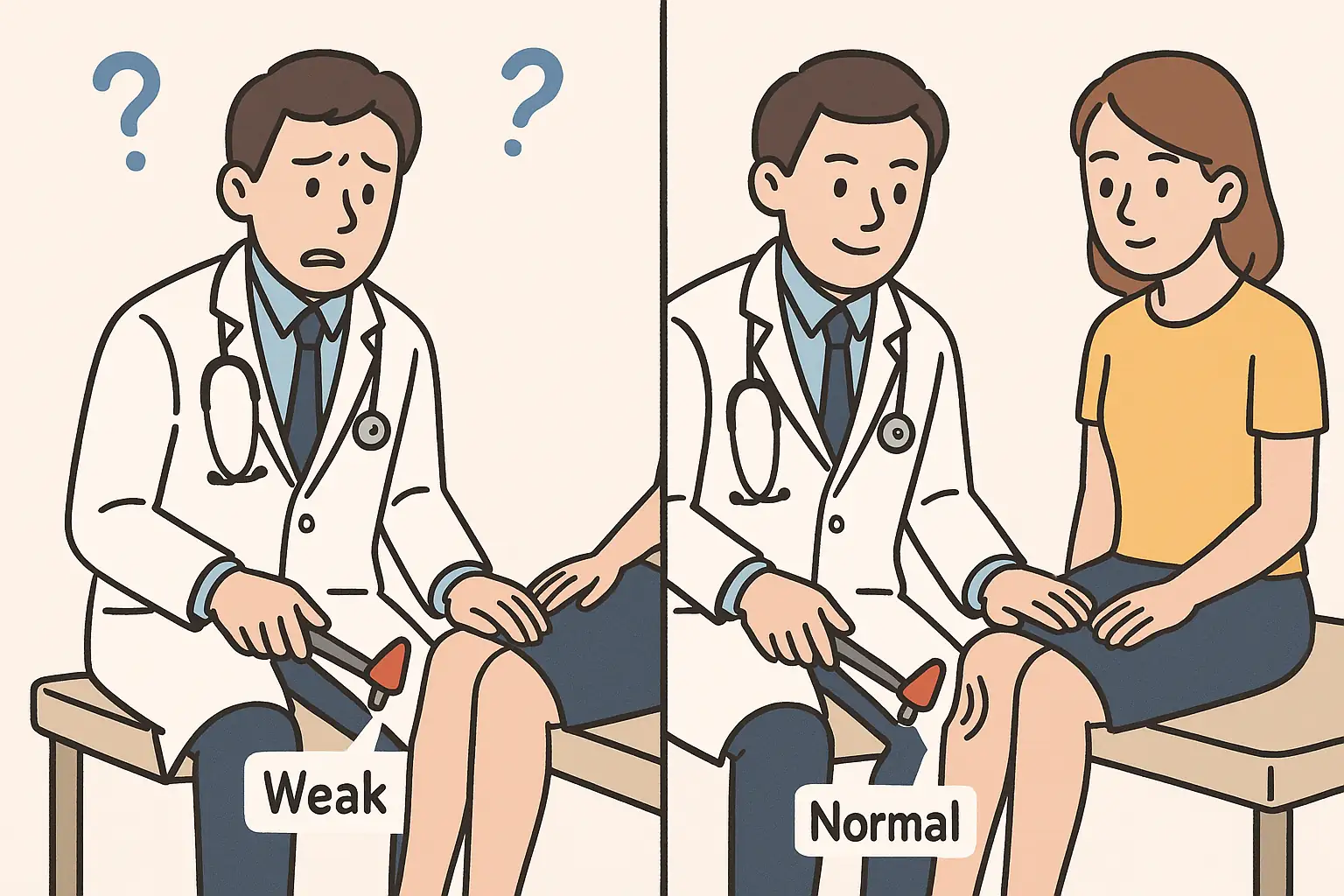
- The patient’s reported weakness seemed to wax and wane.
- On repeating the examination casually (while distracting her with conversation), the weakness disappeared and reflexes returned to normal.
- The patient herself stated: “My legs feel very weak and they wobble every time I try to stand or walk, so I need support from another person to walk.”
- Strikingly, her symptoms seemed to exaggerate when medical staff were present and observing her.
- Despite inconsistencies, the team prioritised patient safety:
- GBS protocol was initiated
- ICU admission arranged for close monitoring (given the risk of sudden respiratory failure)
- Consultant’s impression: “Something just doesn’t add up about this case.”
- The consultant also reviewed investigations done abroad:
- No significant abnormalities
- But felt further evaluation was still needed
Examination Findings
The patient underwent a detailed clinical examination.
- Consciousness & orientation: Patient was alert and oriented to time, place, and person
- Vitals: Stable (BP and pulse rate normal)
- General survey:
- No pallor
- No icterus
- No cyanosis
- No clubbing
- No lymphadenopathy
- Skin, hair, nails: Normal
- Higher mental functions: Normal
- Cranial nerves: Intact
- Deep tendon reflexes:
- Ankle jerk & knee jerk diminished bilaterally (R > L) during the initial examination
- Reflexes returned to normal on repeat testing
- Findings were inconsistent across examinations
- Gait: Wobbly, patient required support to stand
- Arm strength: Normal power
Patient initially reported a mild reduction in sensation below both knees
In neurological emergencies, discussions around escalation of care and DNAR decisions may also come into play.
Initial Assessment & Results
- The patient was admitted to the ICU for continuous observation, primarily to monitor for:
- Respiratory compromise
- Diaphragmatic weakness (a feared complication of GBS)
- Single breath count test was performed at intervals → no decline in respiratory function noted
- Blood investigations: Largely unremarkable
- Early GBS can present with normal blood results, but:
- Absence of inflammatory markers
- No electrolyte disturbances
- These findings strengthened the consultant’s suspicion that something didn’t fit
- Nerve Conduction Studies (NCS) & Electromyography (EMG):
- No definitive signs of demyelination or axonal damage (expected in GBS)
- Only mild, ambiguous changes → could represent very early disease, but also non-specific
- Lumbar puncture / CSF analysis:
- Normal findings
- No albuminocytological dissociation (classically seen in GBS: high protein, normal cells)
- Summary: The “classic” GBS picture dissolved.
- Despite an intensive work-up, the findings were equivocal
- The consultant noted:
- The inconsistencies were becoming more pronounced
- Suggested the case might have a psychological component
- Recommended revisiting history with a focus on medications and family background
The Diagnostic Labyrinth: Investigations & Mimics
When faced with a case where the history strongly suggests GBS but the investigations are inconclusive, we must carefully rule out both GBS and its mimics.
Key Diagnostic Investigations
- Classic GBS finding: albuminocytological dissociation (↑ protein, normal WCC).
- Caveat: CSF can be normal in the first week of illness.
- Alternative clue: A significant WCC (>50 cells/µL) suggests infection or inflammation (e.g., viral meningitis, Lyme disease, myelitis).
- Assess electrical conduction in nerves and muscle activity.
- In GBS: slowing, conduction block, or reduced muscle response.
- Limitations: May be normal early on, requiring repeat testing.
- Patient’s results: Mild, non-specific changes only.
- Routine: CBC, electrolytes, renal & liver function tests.
- Specific causes:
- Hypokalemia → sudden paralysis mimic
- Antibody tests (e.g., anti-GQ1b for Miller Fisher syndrome, a GBS variant)
- Note: Negative antibodies don’t exclude GBS.
- Excludes other conditions:
- Spinal cord compression (tumour, abscess, disc herniation)
- Acute transverse myelitis
- In GBS, sometimes a subtle enhancement of nerve roots, but it is not always present.
Some presentations blur the line between psychiatry and neurology — for example, certain delusional states can mimic physical illness.
Differential Diagnoses Considered
| Category | Examples / Notes |
|---|---|
| Neuromuscular junction disorders | – Myasthenia gravis – Lambert–Eaton syndrome |
| Toxins & Infections | – Botulism (toxin-mediated) – Tick paralysis – Heavy metal or radiation exposure – Certain medications |
| Spinal cord disorders | – Acute transverse myelitis – Spinal cord compression (surgical emergency) |
| Metabolic / Electrolyte issues | – Severe hypokalemia → sudden paralysis, often GI-triggered |
| Muscle disorders & rare causes | – Myopathies – Porphyria (rare but possible) |
Unveiling the Truth: The Psychosocial Dimension
After extensive testing for rare neurological conditions, all results continued to return negative. Our consultant still felt the picture was incomplete. He sensed the family might be withholding crucial information.
Family Dynamics Observed
- Patient was accompanied by:
- Sister
- Mother
- Brother
- One-year-old child
- Consultant noted the absence of the husband, despite the patient being married.
Private Family Discussion
The consultant approached the family empathetically and calmly, avoiding accusations. This careful approach uncovered hidden details:
- Had stopped them completely at times
- Patient’s married life was strained.
- The stress worsened after the birth of her child.
- She had previously been diagnosed with anxiety and depression.
- She had undergone Cognitive Behavioural Therapy (CBT) but did not complete it.
- She was on antidepressant medication, but:
- Took them irregularly
- Had stopped them completely at times
Why Was This Hidden?
- Cultural and religious stigma
- Desire to protect the patient’s privacy
- Family initially presented only the physical complaints
Clinical Reflection
- It is not uncommon for psychological stress to manifest as physical symptoms.
- This phenomenon, known as somatisation, occurs when emotional pain is expressed through bodily complaints.
- The consultant’s hypothesis solidified:
- This was not Guillain-Barré Syndrome
- Instead, it was a somatoform (conversion) disorder

The Placebo Effect & Path Forward
With serious physical causes ruled out and suspicion of a non-organic disorder high, the consultant decided to use a placebo test — applied carefully, ethically, and with family awareness.
Step Taken
- The patient was informed she would receive a “new powerful medication” for her weakness.
- In reality, she was given a normal saline IV bolus, administered twice daily.
Clinical Response
- After first dose:
- Weakness improved
- She was able to stand on her own feet by evening
- Within one day:
- Moving more freely
- Engaging more with staff and family
- Notable inconsistency:
- Appeared worse when doctors were observing
- Appeared better when unobserved (confirmed by nursing staff)
Diagnostic Confirmation
- This rapid improvement with a placebo strongly supported the hypothesis of a conversion disorder rather than Guillain-Barré Syndrome.
Shift in Management Plan
- Focus moved away from a neurological emergency toward a psychiatric and psychological approach:
- Comprehensive psychiatric consultation
- Counseling & psychotherapy
- Consideration of safe antidepressant therapy (as the patient was breastfeeding)
- Involvement of family in ongoing care
Management Plan & Outcome
Reorientation of Care
After 2 days of placebo and rapid symptom improvement, the management focus shifted:
- From a neurological emergency
- To a psychiatric and psychosocial approach
Psychiatric Involvement
- Psychiatric consultation performed
- Long-term plan included:
- Counseling
- Psychotherapy
- Possible medication for underlying anxiety/depression (with breastfeeding safety considered)
Family Concerns
- Relatives were initially uneasy about discharge:
- Worried symptoms would recur outside the hospital
- Solution:
- Patient received counselling about her condition
- Option of a voluntary psychiatric hold was offered, allowing her to continue treatment in a safe setting
Patient’s Progress
- After nearly a week in hospital:
- Clinically improved
- Mentally more stable
- Acknowledged her diagnosis and expressed desire to improve for herself and her child
- Showed readiness to engage in long-term therapy
- Family agreed to support her ongoing journey
Multidisciplinary Effort
The case involved collaboration across multiple specialities (MDT):
- Emergency Medicine
- Neurology
- Psychiatry
- Clinical Psychology
- Nursing staff
Conclusion: The Art of Holistic Diagnosis
This case of a 37-year-old female was a huge learning experience for our entire team.
Case at a Glance
| Aspect | Details |
|---|---|
| Patient | 37-year-old female |
| Presentation | 1 week of progressive bilateral leg weakness, after fever & gastroenteritis |
| Initial Impression | Classic Guillain-Barré Syndrome (GBS) → admitted to ICU |
| Examination | – Reflexes: Inconsistent (sometimes reduced, sometimes normal) – Gait: Wobbly, needed support – Sensation: Mildly reduced below knees |
| Investigations | – Bloods: Normal – NCS/EMG: Mild, non-specific changes – CSF: Normal (no albuminocytological dissociation) – MRI: No cord compression or myelitis |
| Differentials | – GBS & variants – Myasthenia gravis, Lambert-Eaton – Botulism, tick paralysis, toxins – Spinal cord pathology – Hypokalemia, myopathies, porphyria |
| Turning Point | – Symptoms fluctuated depending on observation – Family revealed hidden psychiatric history & stressors – Placebo (IV saline) → rapid improvement |
| Final Diagnosis | Conversion disorder (somatoform disorder) |
| Management | – Multidisciplinary: Neurology, Psychiatry, Psychology, Nursing – Counseling, psychotherapy, antidepressant review – Family involvement |
| Key Lesson | – Multidisciplinary: Neurology, Psychiatry, Psychology, Nursing – Counselling, psychotherapy, antidepressant review – Family involvement |
Key Takeaways
- Began as a neurological emergency (suspected Guillain-Barré Syndrome)
- Ultimately unfolded as a complex case of psychosocial distress manifesting as physical symptoms (conversion disorder)
- Reinforced the importance of clinical observation and careful history-taking
- Highlighted the mind–body connection in medicine
- Emergencies like GBS underscore the importance of junior doctors being ALS certified and prepared for acute deterioration.
Why This Matters
- Classic symptoms don’t always mean a classic diagnosis
- True healing often requires:
- Looking beyond the physical complaint
- Understanding emotional, social, and psychological dimensions
- Each patient brings a unique story that can reshape the entire clinical picture
Memorable Quotes to Reflect On
- “A good physician treats the disease. A great physician treats the patient who has the disease.” – William Osler
- “It is more important to know what sort of person has a disease than to know what sort of disease a person has.” – Hippocrates
Final Reflection
The frequent overlaps between psychiatric and neurological conditions remind us of the complexity of medicine. This case was a powerful reminder that:
- Care requires time, patience, and empathy
- Sometimes, the most challenging diagnosis is not about finding a rare disease, but about understanding the intricate interplay between the mind and body
- The most effective treatment often begins with something simple: truly listening