As a junior doctor, one of the most frequent challenges you’ll face on the wards is Acute Kidney Injury (AKI).
It can develop in any speciality — from a frail medical patient with diarrhoea to a post-operative surgical patient struggling with sepsis.
Recognising AKI stages is crucial, not only for prompt management but also for deciding when to escalate care. This guide is designed as a practical bedside reference for juniors.
We’ll cover the definition of AKI, how to spot the AKI warning stage, causes, the different stages of severity, complications, investigations, and management principles. By the end, you should feel more confident in recognising and managing AKI safely.
What is Acute Kidney Injury
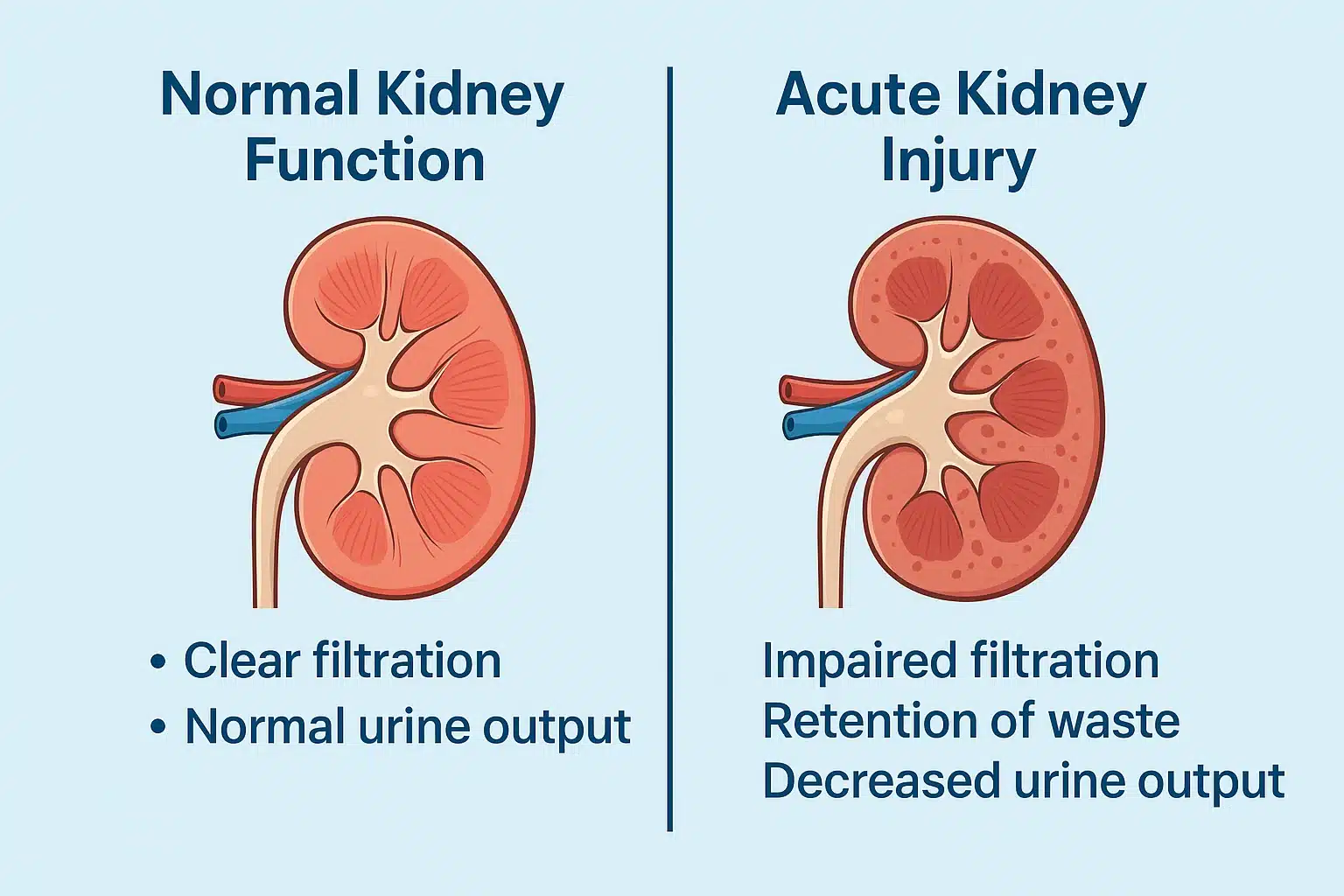
Acute kidney injury is defined as a sudden reduction in kidney function occurring over hours to days.
This results in the retention of waste products (such as urea and creatinine), disturbances in electrolyte balance, and fluid imbalance. According to KDIGO (Kidney Disease: Improving Global Outcomes):
- An increase in serum creatinine by ≥26.5 μmol/L within 48 hours, OR
- An increase to ≥1.5 times baseline within 7 days, OR
- A urine output of <0.5 mL/kg/hour for >6 hours
Why it matters clinically:
- AKI is seen in up to 1 in 5 inpatients.
- Mortality ranges from 20% to 50% depending on severity, especially in the ICU.
- It’s a significant risk factor for long-term chronic kidney disease (CKD).
Recognising the AKI Warning Stage
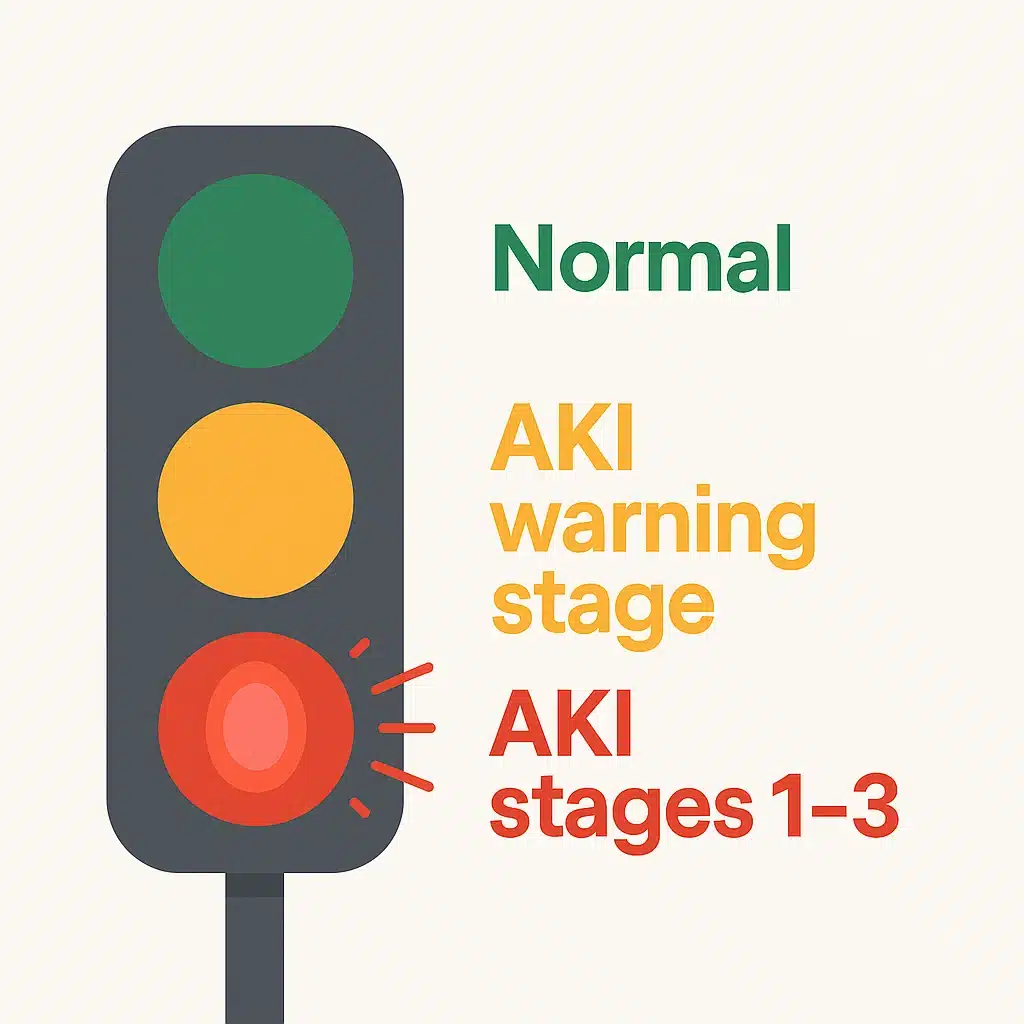
Before patients meet formal KDIGO criteria for AKI stage 1, they often sit in a warning stage. This is an opportunity to intervene early.
Clues that a patient is in the AKI warning stage:
- Declining urine output over 6–12 hours, even if still measurable
- A small but rising creatinine trend (not yet 1.5 × baseline)
- Patients with sepsis, hypotension, or dehydration who are on nephrotoxic drugs
- Elderly or comorbid patients with CKD, diabetes, or heart failure
- Recent contrast exposure in a high-risk patient
Why it matters:
- Identifying this stage allows you to stop nephrotoxins, administer fluids, and treat the infection.
- Documenting “at risk of AKI” prompts closer nursing monitoring.
- Prevents progression to AKI stage 1, stage 2, or stage 3.
Ignoring warning signs can quickly escalate to full-blown AKI, often requiring complex management.
Doing ALS becomes mandatory if you are frequently on-call and see sick patients.
Causes of Acute Kidney Injury
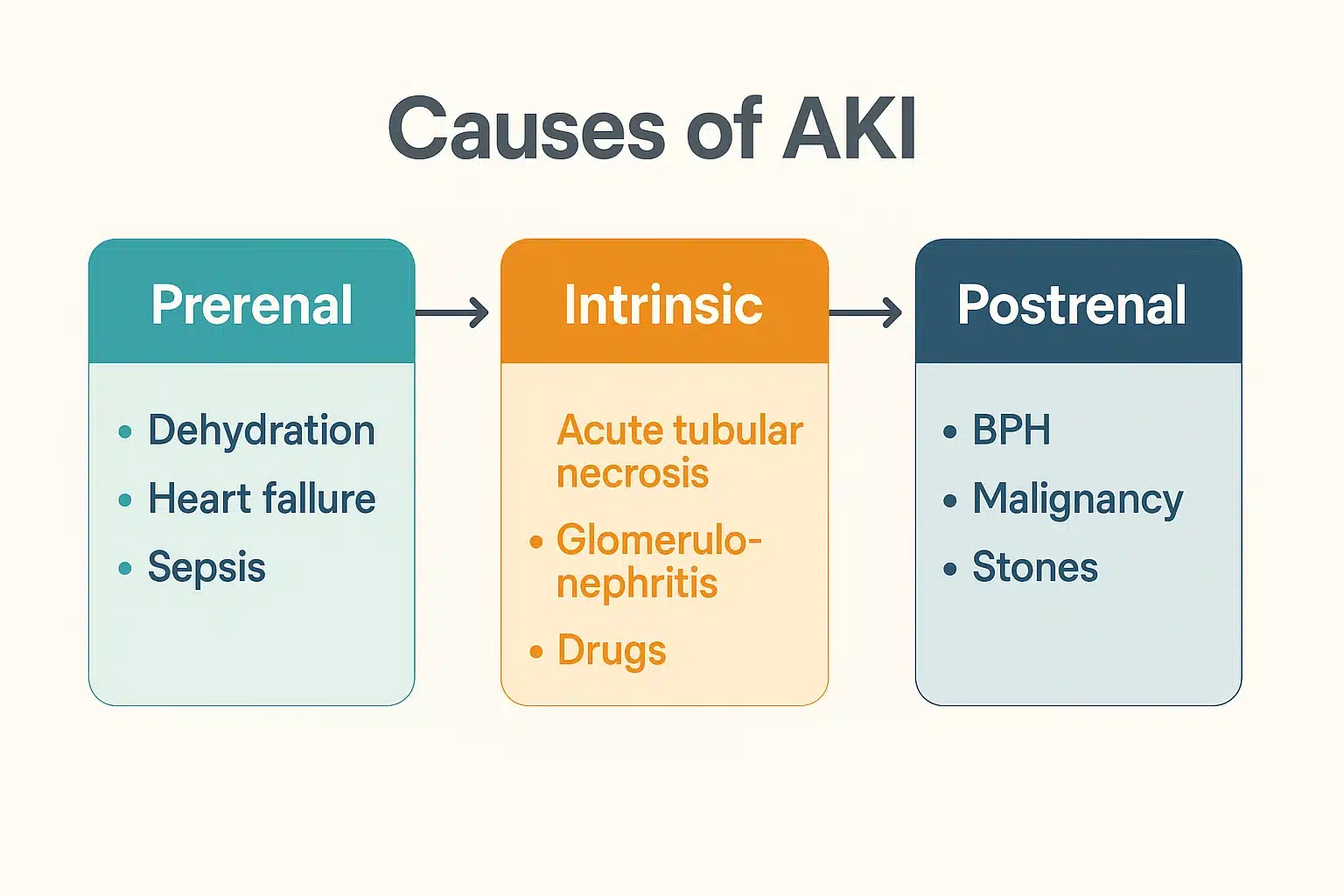
You’ll often hear AKI described as prerenal, intrinsic, or postrenal:
Prerenal (most common)
- Volume depletion: haemorrhage, diarrhoea, vomiting, burns
- Sepsis with poor perfusion
- Hypotension or cardiogenic shock
- Medications: NSAIDs, ACE inhibitors, ARBs
Intrinsic (damage within the kidney)
- Acute tubular necrosis (the most common intrinsic cause)
- Glomerulonephritis (autoimmune or infection-related)
- Interstitial nephritis (often drug-related, e.g. PPIs, NSAIDs, antibiotics)
- Vasculitis, thrombotic microangiopathy
- Nephrotoxins: aminoglycosides, contrast media, chemotherapy
Postrenal (obstruction of urine flow)
- Prostate disease: BPH, cancer
- Stones or ureteric strictures
- Pelvic masses, retroperitoneal fibrosis
- Blocked catheter
AKI Stages Explained (KDIGO Criteria)
Understanding Aki staging is essential for guiding management.
| Stage | Creatinine Criteria | Urine Output Criteria | Clinical Meaning |
|---|---|---|---|
| Stage 1 | ↑ ≥26.5 μmol/L in 48h OR 1.5–1.9 × baseline | <0.5 mL/kg/h for 6–12h | Mild AKI, often reversible |
| Stage 2 | 2.0–2.9 × baseline | <0.5 mL/kg/h for ≥12h | Moderate AKI, higher complication risk |
| Stage 3 | 3 × baseline OR ≥354 μmol/L OR dialysis started | <0.3 mL/kg/h ≥24h OR anuria ≥12h | Severe AKI, often requires dialysis |
Practical Tips for Juniors
- Always compare creatinine to a baseline if available.
- Don’t forget to check urine output trends.
- Stage 3 AKI is a red flag → call the renal team early.
- Even stage 1 AKI should trigger a management plan and monitoring.
Complications of AKI
As patients progress through the AKI stages, complications become more likely:
- Hyperkalaemia → arrhythmias, cardiac arrest
- Fluid overload → pulmonary oedema, hypoxia
- Metabolic acidosis → shock, confusion, tachypnoea
- Uraemia → pericarditis, encephalopathy, confusion
- Progression to CKD → long-term morbidity and mortality
Assessment & Investigations
History
- Recent illness: vomiting, diarrhoea, sepsis
- LUTS: poor flow, retention, flank pain
- Medications: NSAIDs, ACE inhibitors, aminoglycosides, PPIs
- Risk factors: CKD, diabetes, >65y, peri-operative
It is a good idea to discuss DNAR early with the patient/ family/ NOK if they are very frail and have significant underlying medical comorbidities.
Examination
- BP, pulse, JVP
- Signs of hypovolaemia: dry mucous membranes, reduced skin turgor
- Signs of overload: oedema, crackles
- Palpable bladder or prostate enlargement
Investigations
- Bloods: U&E, bicarbonate, calcium, phosphate, FBC, CRP
- Urinalysis: blood, protein, nitrites, casts
- Imaging: bladder scan, renal ultrasound, CT KUB if obstruction suspected
Using Ultrasound in AKI Assessment
Blood tests and urine output are essential for AKI staging, but imaging often provides the missing piece.
A renal ultrasound helps identify structural causes and can point towards the underlying mechanism of acute kidney injury.
Here’s how to interpret the common patterns:
1. Increased Echogenicity
- Decreased renal length and thin cortex → usually suggests chronic kidney disease (CKD).
- Loss of corticomedullary differentiation and reduced movement with respiration → points towards acute tubular necrosis (ATN).
- Rule out infiltrative causes such as multiple myeloma, amyloid, or deposition diseases.
- Sparse arterial/venous flow to the kidney on Doppler → think renal vein thrombosis.
2. Normal Echogenicity
If the kidneys look structurally normal, turn your attention to circulation:
- Flat IVC, low JVP, collapsible ventricles → suggests intravascular depletion (dehydration, sepsis).
- IVC enlarged and not collapsible, raised JVP, venous congestion on VExUS → impaired perfusion from cardiac failure or fluid overload.
- Dilated ventricles, reduced function, pericardial effusion → may indicate cardiorenal syndrome (CRS).
- Features of cirrhosis with ascites and portal venous flow reversal → consider hepatorenal syndrome (HRS).
3. Hypoechoic Kidneys
- Diffuse changes → think cortical necrosis.
- Localised hypoechoic areas → possible renal infarction.
4. Hydronephrosis
- Strongly suggests postrenal AKI due to obstruction.
- Next steps: assess bladder outlet, check catheter position, and exclude physiological hydronephrosis.
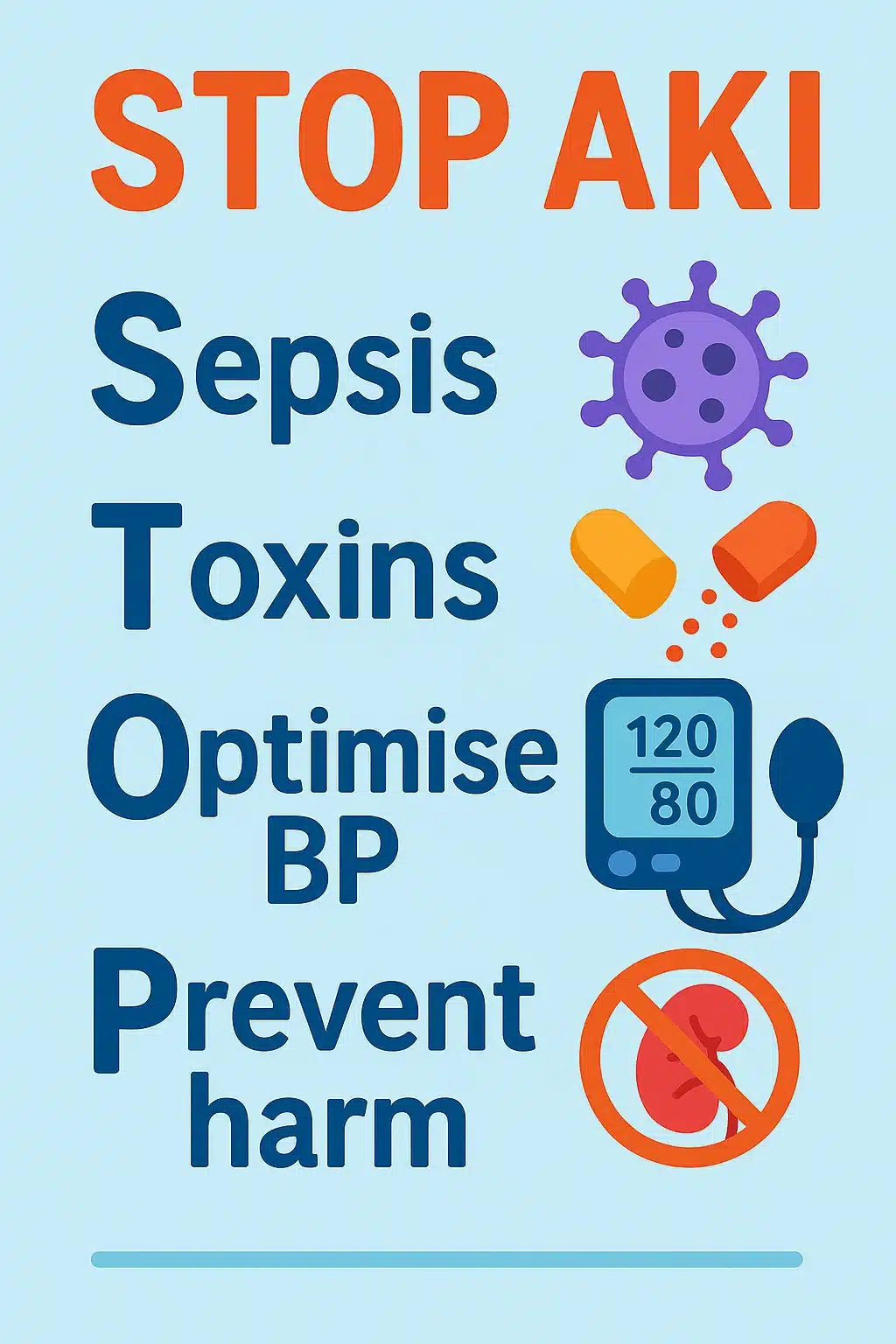
Initial Management Principles
When you diagnose AKI, think STOP AKI:
- S – Sepsis: Identify the source and treat promptly (antibiotics, source control).
- T – Toxins: Avoid nephrotoxic drugs (NSAIDs, ACE inhibitors, ARBs, aminoglycosides, contrast).
- O – Optimise BP/Volume: Rehydrate the patient if hypovolaemic, support blood pressure, avoid overload.
- P – Prevent Harm: Monitor electrolytes, manage hyperkalaemia/acidaemia, review drug doses, and ensure fluid balance is correct.
Do not forget to adjust VTE prophylaxis for the patient if they have AKI.
This should be done by calculating creatinine clearance and eGFR and adjusting according to local trust guidelines.
Other Measures
- Insert a urinary catheter if the urine output is unclear
- Daily weights and strict fluid balance
- Monitor blood daily until improvement
- Escalate early if worsening or not improving
Managing Complications
- Hyperkalaemia:
- ECG monitoring
- Calcium gluconate to stabilise the myocardium
- Insulin + dextrose, nebulised salbutamol to shift K+
- Dialysis if refractory
- Fluid overload:
- Restrict fluids, give IV furosemide if responsive
- Dialysis if resistant
- Metabolic acidosis:
- Treat the underlying cause
- Sodium bicarbonate if severe and pH <7.1
- Dialysis if refractory
- Uraemia:
- Dialysis for encephalopathy, pericarditis, and severe symptoms
Make sure the patient has a patent cannula, as aggressive fluid management may become necessary.
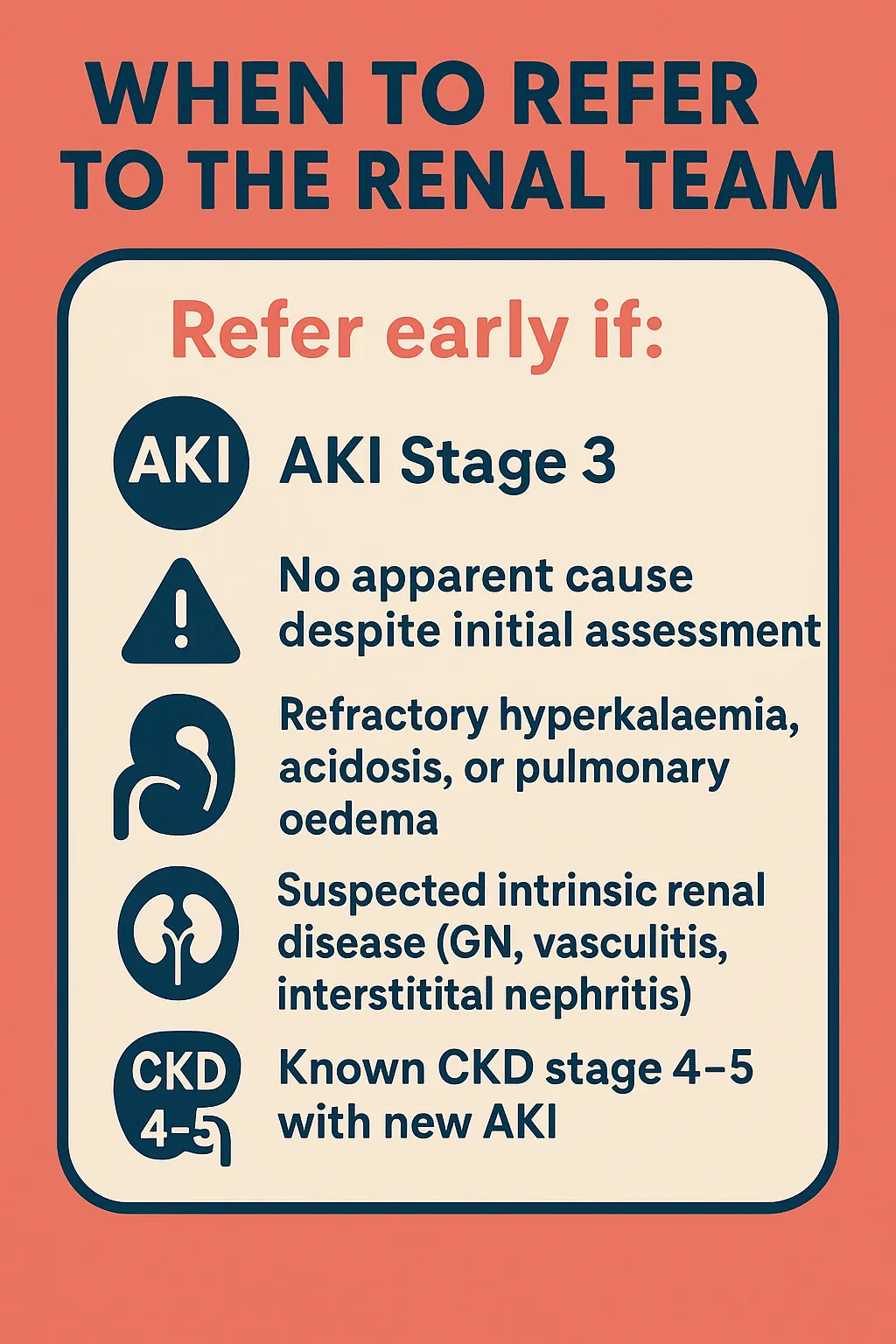
When to Refer to the Renal Team
Refer early if:
- AKI Stage 3
- No apparent cause despite initial assessment
- Refractory hyperkalaemia, acidosis, or pulmonary oedema
- Suspected intrinsic renal disease (GN, vasculitis, interstitial nephritis)
- Known CKD stage 4–5 with new AKI
Summary: Key Takeaways for Juniors
- Acute kidney injury is common and serious — recognise early.
- AKI warning stage is your chance to prevent progression.
- AKI staging is based on creatinine and urine output.
- AKI stage 1 = early but needs action, AKI stage 2 = moderate risk, AKI stage 3 = severe and often requires renal input.
- Complications kill → check potassium, volume status, and acidosis.
- Use STOP AKI for initial management.
- Always escalate AKI stage 3 or refractory complications.