If you’re a junior doctor or IMG starting in the NHS, one of the first things you’ll encounter is the bleep. What is a bleep in the NHS? Simply put, it’s a pager system still widely used across UK hospitals.
The NHS bleep system alerts doctors with a loud tone and displays a callback number. No texts, no apps—just a noise that says, “Call back now.” While it may feel old-school, it remains reliable because it doesn’t rely on Wi-Fi or mobile signal, working even in hospital basements.
Despite newer messaging platforms, the NHS pager system is far from extinct. Learning how to use a bleep is part of everyday life for FY1s, SHOs, registrars, and IMGs alike. From routine patient reviews to emergencies, the bleep keeps the hospital connected.

It might seem intimidating at first—especially with its sudden, loud sound—but once you get used to it, it becomes just another part of the on call shift.
If you’re preparing for NHS interviews as a junior doctor or IMG, check out The Complete NHS Interview Questions Guide with Templates.
How the NHS Bleep System Works
What Happens When You Get Bleeped

When your NHS bleep system goes off, here’s what typically happens:
- You’ll hear a loud tone from the pager.
- A number appears on the screen — this is the callback extension.
- No patient name, task, or urgency details are shown — only the number.
Why It’s One-Way Communication
- NHS Bleeps are designed for reliability and simplicity.
- Only the callback number shows to keep things quick and secure.
- You must call back to find out what’s needed.
Callback Process Example
- Your bleep goes off showing: 70123.
- You find a hospital phone and dial 70123.
- You say: “Hello, this is Dr [Your Name], returning a bleep for extension 70123.”
- The person explains the reason — e.g., “We need you to review Mr Khan in bed 4.”
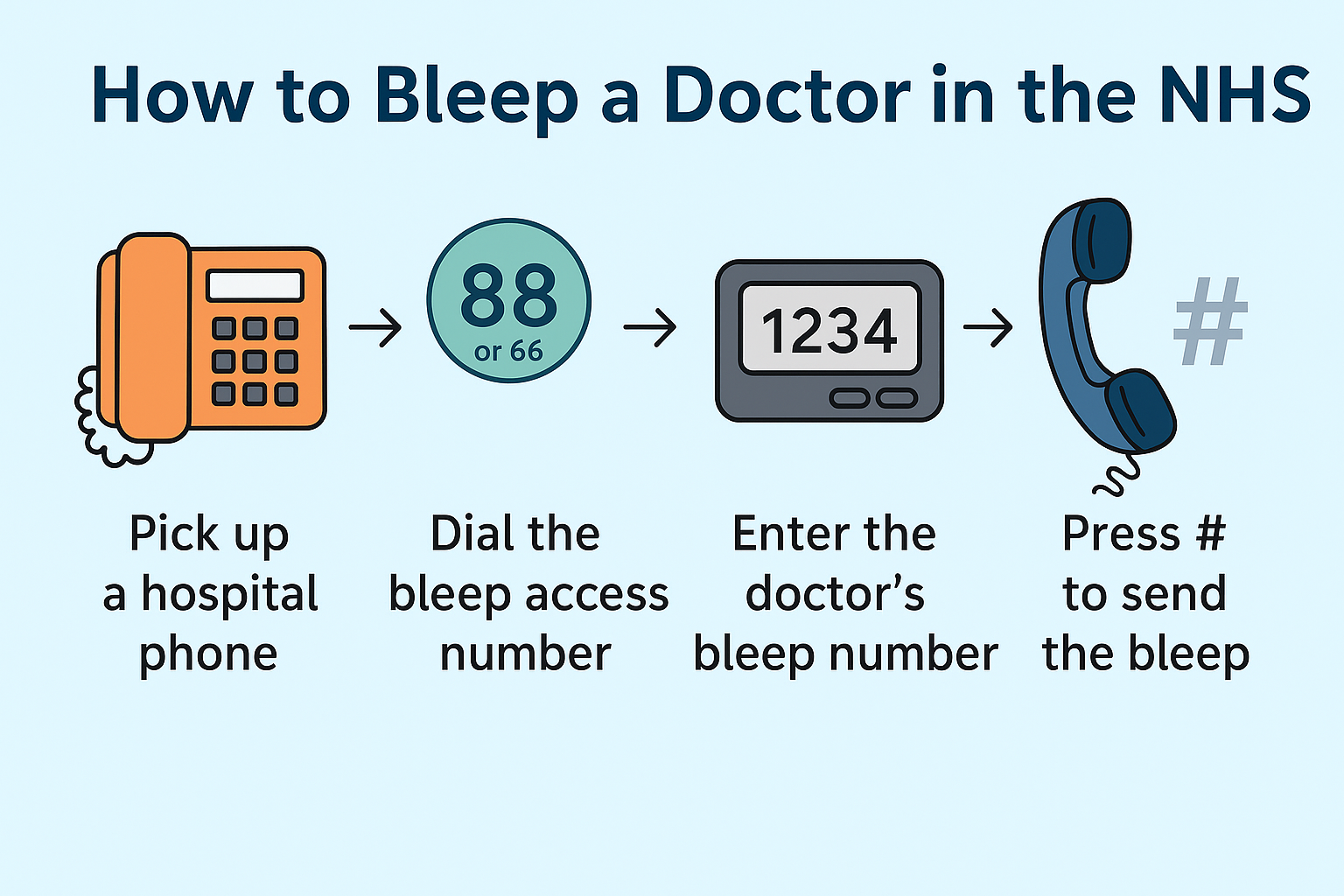
How to Bleep a Doctor in the NHS: Step-by-Step Process
Step 1
Find a hospital landline phone — usually at ward desks, doctors’ rooms, or nurses’ stations.
Step 2
Dial the hospital’s bleep access number (commonly 88, 66, or a specific 4-digit code depending on the trust).
Step 3
Enter the bleep number of the doctor you want to contact. Each role or department has a specific assigned number.
Step 4
Enter your phone extension number when prompted so they know where to call back.
Step 5
Press # (or follow system instructions) to send the bleep.
Step 6
Stay by the phone for at least 5 minutes to wait for the callback.
Common Bleep Access Numbers
- Most hospitals use 88 or 66.
- Check the local directory or induction app for the correct number.
- Always stay by your phone after sending a bleep, especially for urgent requests.
Looking for tips on landing NHS jobs? Here’s Best 5 Places to Look for NHS Jobs that IMGs and UK graduates find useful.
Who Carries Bleeps in NHS Hospitals?
In the NHS, not every staff member carries a pager. The NHS bleep system is primarily designed for medical staff who need to be reachable while moving around the hospital.
Foundation Year 1 (FY1) doctors often carry bleeps for ward cover and patient reviews, while adjusting to new responsibilities and understanding NHS pay structures.

Junior Doctors: FY1, FY2, and SHOs
- Foundation Year 1 (FY1) doctors often carry bleeps for ward cover and patient reviews.
- Foundation Year 2 (FY2) doctors and SHOs (Senior House Officers) usually have additional responsibilities like reviewing deteriorating patients or taking referrals, so carrying it becomes routine.
- During on-call shifts, FY1s and SHOs are assigned specific ones covering either wards or the whole hospital depending on rota arrangements.
Registrars and Consultants
- Medical registrars (IMT and specialty registrars) carry specific NHS bleep numbers as the senior decision-makers for acutely unwell patients.
- Registrars are typically bleeped for MET (Medical Emergency Team) calls, referrals from other specialties, and serious patient deterioration.
- Consultants may have it while on-call but often rely on mobile phones or switchboard transfers outside working hours.
Specialist Roles and Departments
Some hospital departments carry dedicated NHS bleeps for service coordination:
- Radiology: For urgent scan requests or result discussions.
- Pharmacy: For medication queries, particularly out-of-hours drug availability.
- Porters, estates, and security teams: May also use pager systems separate from clinical roles.
Baton Bleep System Explained
- A baton bleep isn’t assigned to a single person but to a role or shift.
- For example, “Medical SHO bleep 1234” is passed from the day doctor to the night doctor at handover.
- This ensures continuity: whoever holds the baton ones are responsible for responding during their shift.

For structured application help, here’s Trac Jobs NHS Application Guide with Templates for Doctors.
Practical Guide: How to Use a Bleep
For junior doctors and IMGs starting in the NHS, knowing how to use a NHS bleep system properly is part of everyday survival.
The NHS bleep system may seem basic, but there’s a right way to handle your pager to avoid missing urgent requests or causing unnecessary delays.
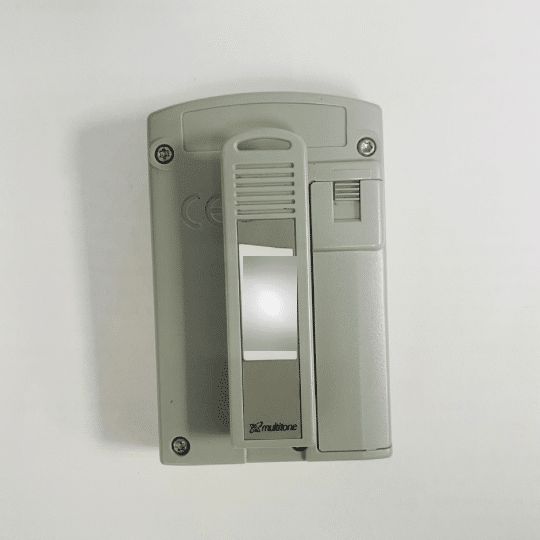
Collecting Your Bleep
- Always collect your assigned bleep at the start of your shift from handover room or switchboard or your department’s admin desk.
- Check that it’s switched on and working. Some doctors test it by asking a colleague to send a trial bleep.
- Make a note of your pager number—it’s often written on the back of the device as well.
Turning It On and Adjusting Volume
- Switch the NHS bleep on using the power button or side switch.
- Adjust the volume to ensure it’s loud enough to hear over ward noise. Hospitals can be busy and noisy, so keeping your pager on silent is only for rare situations (like during a procedure or teaching session).
- Vibrate mode is available on some models but isn’t standard on all NHS pagers.
Silencing and Vibration Settings
- If you’re in a sensitive environment—breaking bad news or attending a quiet teaching session—you can silence your bleep temporarily.
- Always remember to turn the volume back on immediately afterward.
- Missing bleeps because the volume was left off can delay patient care and affect your team’s workflow.

Checking Missed or Stored Bleeps
- Most NHS pagers store the last few numbers that bleeped you.
- If you’ve been away from your pager (for example, while scrubbed in theatre), check the screen for any missed calls.
- Always return missed bleeps promptly. It’s part of good bleep etiquette and patient safety.
Managing Batteries
- NHS bleep system usually run on AA or AAA batteries.
- Battery life varies depending on the model and volume settings, but it’s good practice to replace the battery at least once a week.
- Spare batteries are available from switchboard, porters, or ward stock rooms. Never assume the bleep will last all week—check regularly to avoid your pager dying mid-shift.
Troubleshooting Common Issues
- If your pager is faulty (not sounding, blank screen, constant error tone), report it to switchboard.
- They’ll either replace it or check if there’s a system-wide issue.
- Always let your team know if your bleep is out of action, even temporarily, so you can be contacted via another method if needed.
And if you’re also preparing for MRCP Part 1 while working full-time, see How I Passed MRCP Part 1 in 2 Months with Full-Time NHS Job.
Types of Bleeps in NHS Hospitals
In NHS hospitals, not all pagers carry the same level of urgency or responsibility.
Understanding the different types of bleeps is essential for junior doctors and IMGs to prioritise tasks effectively and know when immediate action is required.
Routine Ward Bleeps
This is the most common type of NHS bleep system a junior doctor carries. Routine ward pagers cover everyday patient care tasks such as:
- Writing up drug charts or prescriptions
- Reviewing blood test results
- Cannula insertions and venepuncture requests
- Reviewing patient symptoms like low blood pressure or chest pain
While these are important, they are generally non-urgent. Routine ward pagers can come at any time during your shift, and learning how to triage them alongside other tasks is part of ward cover and on-call duty.
Medical Emergency Team (MET) Bleeps
The MET bleep, sometimes called a “2222 bleep” depending on trust policy, is activated when a patient deteriorates rapidly but isn’t yet in cardiac arrest.
It’s issued to senior doctors such as registrars and to specific MET team members.
Common reasons for MET calls include:
- Severe hypoxia
- Seizures
- Acute confusion or reduced consciousness
- Dangerous arrhythmias
If you’re not part of the MET team, it’s good etiquette not to interrupt doctors carrying these pagers unless necessary.

Need NHS indemnity insurance options? Explore Best 5 Medical Indemnity Insurance for UK NHS Doctors.
Crash Team Bleeps (2222 Call)
The crash bleep is reserved for cardiac arrests and other life-threatening emergencies. These are typically carried by:
- ICU registrars
- Medical registrars
- Anaesthetists
- Dedicated resuscitation teams
When a 2222 call goes out, the pager alerts those carrying crash pagers to attend immediately. In most hospitals, crash bleeps have a distinct sound pattern, so they’re easily recognisable even in a busy environment.
Specialist Department NHS Bleeps
Beyond routine and emergency teams, specialist departments also carry dedicated NHS bleeps for service coordination:
- Radiology: for urgent scan requests, reporting delays, or queries about imaging procedures
- Pharmacy: for medication stock checks, clarifications, or out-of-hours drug issues
- Haematology, Oncology, or Surgical specialties may have their own departmental pagers depending on the hospital
Some hospital departments carry dedicated pagers for service coordination, which is especially important in understanding multi-disciplinary teams.
As a junior doctor, you’ll often need to liaise with radiology or pharmacy teams, so becoming familiar with these departmental pagers is part of everyday NHS practice.
Real-World Scenarios Where NHS Bleeps Are Used
Once you start working in the NHS, especially as a junior doctor or IMG, the pager will become a regular part of your day—or night. Whether you’re on a general medical ward, doing nights, or covering surgical lists, understanding when and why you might get bleeped helps you stay organised and prioritise tasks safely.

Urgent Patient Reviews
One of the most common reasons for an NHS bleep is a patient needing review. This could be for:
- Low blood pressure (hypotension)
- High heart rate (tachycardia)
- Oxygen desaturation
- Sudden chest pain
- New-onset confusion
Typically, nurses or healthcare assistants bleep the on-call doctor if they notice a patient’s vital signs are abnormal or if someone suddenly looks unwell.

You’ll get the callback number, contact them, and then attend the patient as soon as possible, prioritising based on clinical urgency.
Prescription and Drug Chart Issues
Another regular scenario is being bleeped for prescribing medication. Common examples include:
- Missing pain relief prescriptions
- Antiemetic (anti-sickness) drugs for patients who feel nauseous
- Stat doses of antibiotics after a positive infection result
- Re-charting medications that have been crossed out or run out
These types aren’t always life-threatening, but they still require timely action—especially if a patient is waiting for pain relief.
Critical Blood Results
Hospital labs will reach doctors directly if they detect critical abnormalities in blood tests. For example:
- Potassium level over 6.0 mmol/L (hyperkalaemia)
- Severe anaemia or thrombocytopenia
- Sodium dangerously high or low

In these cases, the lab may not wait for the ward to pick up results—they’ll contact you via the NHS bleep system to ensure urgent review and management.
Imaging Follow-Ups
Radiology departments may reach you for:
- Confirming whether an urgent CT or MRI is still required
- Clarifying clinical details on a scan request
- Reporting serious findings directly, such as a new pulmonary embolism or brain bleed
When a radiologist bleeps you, it usually means they have something that needs immediate clinical action, so these calls are prioritised highly.
End-of-Shift Handover Tasks
During shift changes, outgoing doctors often pass on important patient updates or pending tasks via NHS bleep. You might hear things like:
- “Please review bed 5 before you leave.”
- “I didn’t get a chance to prescribe fluids for Mr Patel—can you do it?”
This ensures continuity of care, especially when patients have ongoing needs that can’t wait until the next morning.

Knowing how to handle these scenarios calmly and efficiently is key to managing NHS bleep calls. It’s also part of building clinical judgement: knowing what requires an immediate response and what can safely wait while you finish another task.
NHS Bleep Etiquette and Communication Best Practices
When working in the NHS, managing your pager isn’t just about answering it quickly—it’s about handling it professionally and efficiently. Whether you’re a junior doctor or an IMG, understanding bleep etiquette helps maintain smooth hospital workflows and reduces unnecessary stress for everyone involved.
How to Respond to an NHS Bleep
When your pager goes off:
- Find the nearest ward or office phone. Don’t wait too long—respond as soon as possible.
- Dial the number shown on the pager screen.
- Always introduce yourself clearly: “Hello, this is Dr [Your Name], returning a bleep for extension [Number].”
- Be polite and listen carefully to the reason for the bleep.
- Clarify any unclear details, such as patient location, urgency, or specific requests.
Doctors new to the NHS often feel pressure to rush through calls, but taking 30 seconds to confirm important information can save time later.

New to the UK? Here’s Top 5 Bank Accounts You Can Choose As New NHS Staff that are IMG-friendly.
Prioritising Multiple NHS Bleeps
Sometimes, especially on night shifts, you may receive several bleeps at once. Here’s how to handle them:
- Prioritise emergencies first (e.g., MET calls, severely unwell patients).
- Routine ward requests can wait until more urgent issues are managed.
- Write down each bleep number and task so you don’t forget or mix things up.
Many junior doctors carry a small notepad or use hospital-approved apps to keep track of bleeped tasks. This is especially useful for busy shifts with high patient turnover.
How to Bleep a Doctor – Sender Etiquette
When you’re the one sending an NHS bleep, remember:
- Include your callback extension—don’t expect the other doctor to know who’s calling.
- Stay by the phone for at least five minutes after sending a bleep, especially for urgent issues.
- Be clear when speaking. State patient name, location, and the reason for the call.
Avoid bleeping someone multiple times in quick succession unless absolutely necessary. Double bleeping (sending two bleeps in a row) is generally reserved for urgent or emergency situations.
Managing NHS Bleeps Under Pressure
If you feel overwhelmed by bleeps—especially on a busy on-call shift—don’t struggle alone:
- Let your registrar or senior doctor know.
- Share tasks with colleagues if appropriate.
- Use hospital systems like the Hospital at Night team to distribute workload fairly.

Good bleep etiquette is about respecting both the person receiving the bleep and the patient involved. Handling NHS bleeps professionally helps create a more efficient, safer hospital environment for everyone.
Modern Alternatives to the NHS Bleep System
While the traditional NHS bleep system remains in use, many trusts are exploring or adopting modern alternatives to improve communication for junior doctors and IMGs. These newer systems aim to provide clearer information, reduce missed messages, and make hospital workflows smoother without relying solely on one-way pagers.
Induction (Accurx Switch) App
One of the most widely used tools alongside bleeps in NHS hospitals is the Induction app, sometimes known as Accurx Switch.
- It provides an up-to-date directory of bleep numbers, extension numbers, and department contacts.
- Doctors can search for specific roles—like “medical registrar on call”—rather than remembering individual NHS bleep numbers.
- Induction helps when you receive an unfamiliar number and need to check which department or doctor it belongs to.
Doctors can search for specific roles—like “medical registrar on call”—rather than remembering individual pager numbers. Useful tools like these feature in NHS apps.
Medic Bleep and Alertive Apps
Several NHS trusts have trialled smartphone-based messaging platforms such as Medic Bleep and Alertive.
- These apps allow secure, GDPR-compliant messaging between healthcare staff.
- Instead of sending a bleep and waiting by the phone, doctors can send direct text-like messages, attach patient details, or clarify urgency immediately.
- Both apps aim to reduce the inefficiency of one-way communication and avoid unnecessary phone calls.
While promising, full replacement of pagers with these apps is not yet universal across the NHS. However, many hospitals are moving in this direction.
Digital Task Management Tools
Platforms like Infinity Health and similar services are being used in some trusts to replace routine ward NHS bleep communication.
- These systems allow nurses and doctors to assign, accept, and complete clinical tasks digitally.
- For example, rather than bleeping a doctor to request a cannula, a nurse might log the task on the system.
- The doctor sees pending tasks on their phone or computer and completes them in priority order.
This helps reduce interruptive communication and allows more structured task management—something particularly helpful for night teams and Hospital at Night setups.
Secure Messaging Platforms: Pando and Microsoft Teams
Many NHS staff use Pando or Microsoft Teams for non-urgent communication.
- These platforms are NHS-approved and encrypted for patient safety.
- Pando is particularly popular for sending handover information or non-urgent messages to team groups.
- Microsoft Teams is often used for larger team coordination, teaching, and virtual meetings rather than direct clinical requests.
While neither platform replaces the NHS bleep system entirely, they serve as useful add-ons alongside it. But in fact, even bleeps are prone to failures.
Wi-Fi Phones and Vocera Badges
Some NHS trusts have introduced Wi-Fi-connected hospital phones or wearable devices like Vocera badges.
- Vocera badges allow hands-free, voice-activated communication between staff members.
- Wi-Fi phones function like hospital-specific mobile phones, providing clearer, faster contact than pagers.
These technologies are still in trial stages in many areas but reflect the NHS’s ongoing efforts to modernise communication methods.
For now, understanding the NHS bleep system remains essential for junior doctors and IMGs.
But being aware of these modern alternatives can make adapting to different hospitals smoother, especially as more trusts adopt new tools to improve patient care and team efficiency.
Essential Tips for IMG Doctors and NHS New Starters
For international medical graduates (IMGs) and junior doctors beginning their NHS careers, getting used to the NHS bleep system is part of adapting to UK hospital culture.
Starting your journey with clinical attachments? Download Free NHS Clinical Attachment Cover Letter Template in PDF.
While it might feel unfamiliar at first, following a few practical tips can make managing bleeps easier and less stressful.

Day-One Bleep Checklist
On your first day or shift, make sure you:
- Collect your assigned bleep from switchboard or your department’s designated point.
- Test that the bleep is working—ask a colleague to send you a trial bleep if needed.
- Adjust the volume to a level that suits busy ward environments.
- Make a note of your bleep number and save key numbers, such as the on-call registrar’s NHS bleep, in a pocket notebook or phone.
- Download the Induction app to easily look up extension numbers and department bleeps across your hospital.
Managing Bleep Anxiety
It’s completely normal to feel nervous about carrying a bleep, especially during your first few weeks in the NHS.
Many IMGs and UK medical graduates share this experience. Here’s how to keep it manageable:
- Stay calm when the bleep goes off. Remember, not every bleep is an emergency.
- Take a breath, find a phone, and respond methodically—clear communication is more important than speed alone.
- Write down each bleeped task as you go, especially during busy on-call shifts. Many junior doctors carry a small notebook or use approved note-taking apps.
- Prioritise tasks sensibly: if you’re handling something urgent, don’t feel pressured to respond to routine bleeps immediately.
- If you’re overwhelmed by constant bleeps, let your senior know—sharing workload is part of safe NHS practice.
Building Your Own System for Managing Tasks
As you settle into NHS hospital life, you’ll naturally develop your own system for handling NHS bleeps efficiently. Some doctors prefer writing everything down on paper; others use task apps approved by the trust. The key is finding a method that:
- Helps you keep track of what’s been asked and what’s been done.
- Ensures urgent tasks don’t get forgotten in the middle of routine work.
- Makes handovers smoother—especially at the end of long or night shifts.
Mastering the bleep system is about more than just responding quickly. It’s about staying organised, communicating clearly, and ensuring patient care is prioritised appropriately.
Over time, managing your bleep becomes second nature, like checking patient observations or reviewing drug charts.
Conclusion
For junior doctors and IMGs stepping into the NHS, understanding the bleep system isn’t just another formality—it’s a core part of everyday hospital life.
Whether you’re handling routine ward cover, responding to emergencies, or chasing scan results, the NHS bleep system keeps the clinical team connected.
It may seem old-fashioned compared to smartphones, but its reliability, simplicity, and resilience in busy environments make it essential.
From knowing how to use an NHS bleep, following bleep etiquette, and handling multiple calls at once, to exploring modern alternatives like secure messaging apps, learning to manage your bleep confidently is part of becoming an efficient NHS doctor.
The first few weeks may feel overwhelming, especially when your pocket suddenly starts beeping mid-task. But with time, handling bleeps becomes second nature—just another part of the structured, organised rhythm that keeps hospitals running.
Whether you’re chasing down routine prescriptions or rushing to a MET call, mastering the pager system helps you deliver safe patient care and fit smoothly into the NHS workflow.
FAQs
Is the NHS bleep system still used in all UK hospitals?
Yes. Although many trusts are trialling secure messaging apps, nearly all UK hospitals continue to use the NHS pager system, especially for emergency and critical alerts. Many trusts are adopting a hybrid approach—modern apps for routine tasks and pagers reserved for MET or 2222 calls.
Can misplaced bleeps be tracked or located?
Most standard pagers don’t have GPS or tracking. If you misplace one, you usually need to inform switchboard and check lost-and-found areas. Some specialty devices used in labs or estates have tracking features, but not ordinary NHS bleeps.
What if there’s no network coverage—will bleeps still work?
Absolutely. NHS bleeps rely on dedicated radio frequencies, so they work even in Wi-Fi or mobile dead zones like basements and radiology suites. That’s a major reason why the pager system remains crucial in hospitals.
Why can’t they just use smartphones in the NHS instead of bleeps?
Smartphones (or apps like Medic Bleep) can deliver more detailed, two-way messaging. However, hospitals often have weak Wi-Fi in certain areas and phones require charging. Pagers are simple, reliable, long-lasting, and don’t freeze or distract with social apps.
How often should I test my bleep?
It’s good practice to test your bleep at the beginning of each shift. Ask a colleague to send you a test page or do a self-test if the pager allows. Spot-checking every few days helps avoid unexpected failures.
What are the costs and plans for removing bleeps in the NHS?
There’s an ongoing plan to phase out non-emergency pagers by the end of 2021 and replace them with secure messaging. However, critical alerts like crash calls will still use pagers until reliable systems are in place. Funding and infrastructure vary between trusts.
Do bleeps show urgency levels?
No. Standard NHS bleeps do not indicate priority—they simply flash a callback number. This is why “bleep etiquette” is vital: always clarify urgency during the callback, and don’t assume all bleeps are equally urgent.
Can I get a two-way pager?
Yes, two-way “alphanumeric” pagers exist, especially in private hospitals or specialty departments. They allow limited text replies. But most NHS trusts still issue basic numeric pagers.
What should I do if I miss a bleep during theatre or a break?
Check your pager’s recent pages list and call back as soon as possible. If it’s urgent—such as a crash bleep—contact the switchboard immediately to find out the location and ensure help arrives on time.
Will I get trained on using the NHS pager system?
Yes—bleep use is covered during trust induction and departmental orientation. New doctors are typically shown how to collect, test, manage, and troubleshoot bleeps as part of their onboarding process.
How to bleep someone in Hospital?
To bleep someone in a hospital using the NHS bleep system, you follow a simple, structured process:
1. Find a hospital landline phone — usually located at nurses’ stations, doctors’ rooms, or ward offices.
2. Dial the hospital’s bleep access number. This varies by trust but is often something like 88, 66, or a dedicated 4-digit code.
3. Enter the recipient’s bleep number when prompted. Each role or person has a specific bleep number — for example, “Medical SHO on-call” might always be bleep 1234.
4. Enter your extension number so they know where to call back. This is the number of the phone you’re using or another internal extension you’ll be waiting at.
5. Press # or follow the automated instructions to complete the process.
After sending the bleep, stay by the phone for at least 5 minutes so the person can call you back.
A few etiquette points to remember:
1. Only bleep for clinically necessary reasons, especially out of hours.
2. If the matter is urgent (like severe bleeding or cardiac arrhythmia), mention urgency when the person calls back.
3. Always speak clearly and confirm patient details and ward location once the doctor calls you back.
Learning how to bleep a doctor correctly helps keep communication smooth, especially during busy shifts or emergencies.