If you’re a doctor new to the NHS, you’ve probably wondered:
“What exactly happens during an on-call shift?”
You hear terms like clerking, ward cover, night shifts, post-take rounds — but no one really explains what you’ll be doing hour to hour. I had the same questions before starting my first on-call rota.
I learned through experience that NHS on-call shifts are intense but manageable if you know:
- Who’s on your team: Consultant on-call, registrar, SHOs, FY doctors.
- What your actual tasks are: Clerking, ward cover, night duties, chasing results.
- How to manage stress, time, and escalation: Especially as a new doctor adjusting to UK protocols.
In this guide, I’ll break down exactly what happens during NHS on-call shifts, how rota banding pay works, and share practical tips I wish I knew before my first shift.
![[Guide] NHS On-Call Shifts: What Doctors Actually Do 1 giphy 3](https://i0.wp.com/scrubtales.co.uk/wp-content/uploads/giphy-3.gif?fit=480%2C256&ssl=1)
NHS On-Call Pay and Perks: What New Doctors Should Know
Many new doctors ask: “Is doing NHS on-call worth it for the pay?” Realistically, on-call shifts can be tiring, but they do come with financial and professional benefits.
How NHS On-Call Banding Works
- NHS on-call shifts attract additional pay through something called rota banding.
- For most full-time junior doctors, especially those at the IMT and SHO levels, this is typically a 40% or 50% banding on top of their basic salary. Here is a good overview of the earnings of junior doctors in the NHS.
Example:
- FY2 basic pay: ~£37,303/year (2025 update)
- +50% banding for on-calls: Extra ~£18,650/year
- Total: ~£55,950/year (before tax)
Banding percentages vary depending on the rota intensity (nights, weekends, frequency of on-calls).
![[Guide] NHS On-Call Shifts: What Doctors Actually Do 2 giphy 4](https://i0.wp.com/scrubtales.co.uk/wp-content/uploads/giphy-4.gif?fit=398%2C478&ssl=1)
If you are still waiting to land your first NHS job, you might want to check our post on TRAC job applications: Complete Guide with sample PDFs.
Professional Perks Beyond Pay
- Faster clinical learning: Especially in clerking, emergency management, and escalation skills.
- Better MRCP preparation: Real-world exposure helps reinforce exam topics, such as ECGs and ABGs.
- Team integration: On-calls help you build relationships with registrars, consultants, and nursing teams.
- Confidence boosting: No doubt once you are done with the toughest jobs, you start to feel ward is no longer interesting.
While on-call shifts are challenging, they’re also a key part of growing as a confident, independent doctor in the NHS system.
NHS On-Call Team Structure: Who’s Who on Shift
Before starting your first NHS on-call shift, one of the most important things is knowing exactly who is on your team. It is crucial to know different NHS roles as well as you understand the structure better.
Many new doctors feel lost during their early shifts simply because they don’t know who to escalate to or who covers which responsibilities. Here’s how a typical NHS on-call team is structured:
🔹 Consultant On-Call
- Senior-most doctor for major clinical decisions and post-take rounds.
- Usually not physically present overnight, but always contactable via registrar.
🔹 Registrar (Medical Registrar or Med Reg)
- The main point of senior support during on-call shifts.
- Reviews complex cases, accepts referrals, and helps junior doctors make decisions.
- Covers multiple wards and admissions overnight.
🔹 SHOs (Senior House Officers)
Includes:
- IMT1–3 doctors
- ST1–2 doctors in other specialities
- Trust-grade doctors (non-training roles)
SHOs handle most of the clerking, ward cover, and reviewing patients before the registrar’s involvement.
If you are not interested in IMT, maybe GP is the way to go. Check out guide on CREST form: How to Fill with links.
🔹 Foundation Doctors (FY1–FY2)
- FY1: Primarily ward cover, not usually responsible for clerking new patients alone.
- FY2: More independent—clerking, ward cover, and basic escalation expected.
Early Ward Round and Team Introduction
Before each on-call shift, there is usually a team meeting or early ward round where everyone introduces themselves:
- Consultant, registrar, SHOs, and FY1–FY2 doctors all state their name and role.
- This helps doctors and new team members understand who is responsible for what.
- Practical tip: Make sure to speak up confidently during introductions, so the team knows you’re part of the rota.
- I have never seen a clinical observer during on-call shifts, but I believe it is a good thing to explore, for sure. If you have not yet completed a clinical attachment, you can try using our custom clinical attachment cover letters.
![[Guide] NHS On-Call Shifts: What Doctors Actually Do 3 Medical on call team](https://i0.wp.com/scrubtales.co.uk/wp-content/uploads/Medical-on-call-team.png?fit=1536%2C1024&ssl=1)
You are also issued a bleep, as per your role, which you must carry throughout your shift.
What Doctors Actually Do During NHS On-Call Shifts
If you’re new to NHS on-call duties, it’s easy to feel unsure about what your role really involves. On paper, the job description may say clerking, ward cover, and night shifts — but what does that mean in practice?
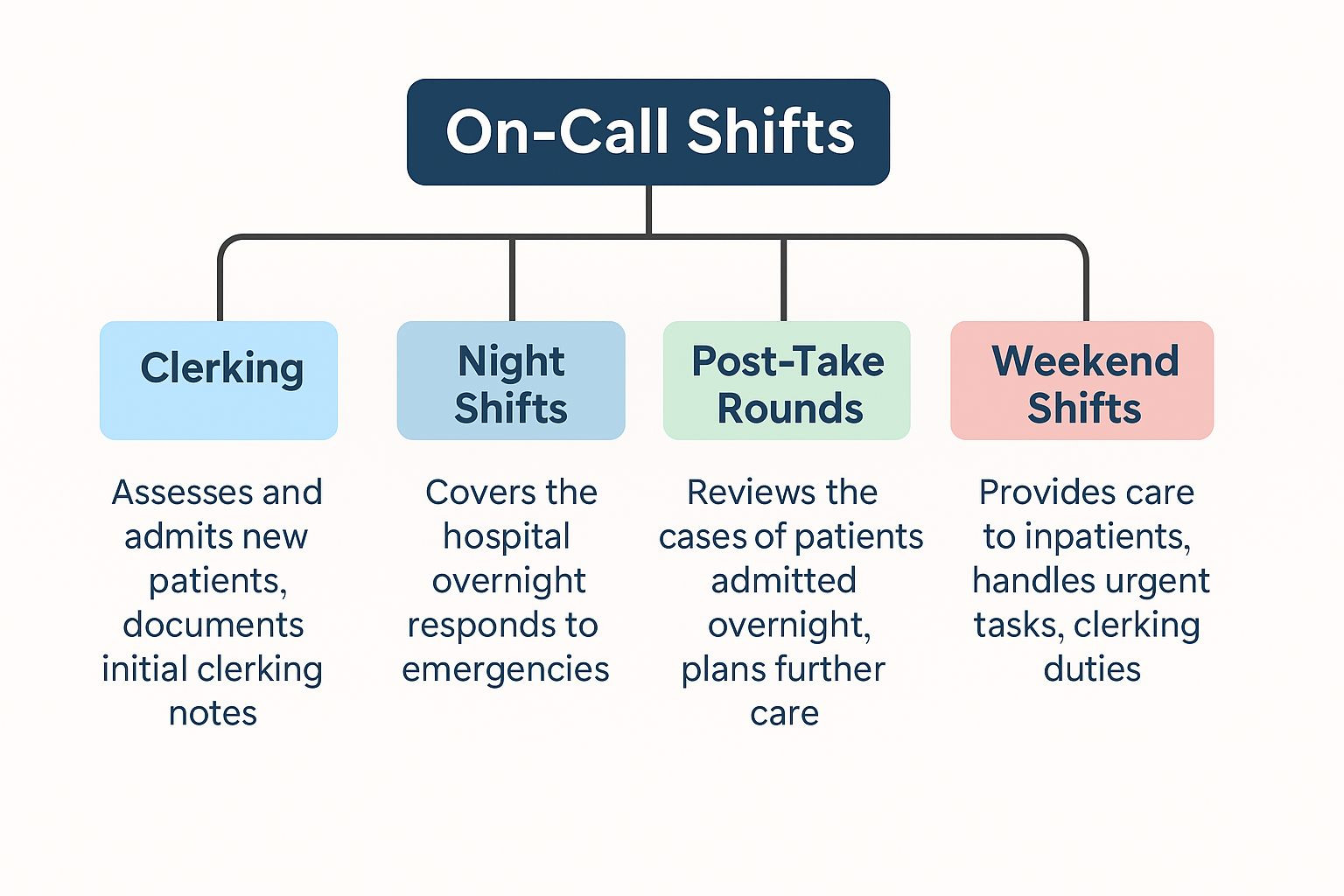
Here’s a breakdown of what junior doctors actually do during NHS on-call shifts:
Clerking New Admissions
![[Guide] NHS On-Call Shifts: What Doctors Actually Do 5 Medical Admissions Clerking proforma](https://i0.wp.com/scrubtales.co.uk/wp-content/uploads/Medical-Admissions-Clerking-proforma.png?fit=1280%2C1811&ssl=1)
One of the key tasks for on-call doctors, especially FY2s, IMT doctors, and SHOs, is clerking new patients. This means:
- Taking a full history and examination
- Ordering blood tests, ECGs, and chest X-rays
- Writing an admission note in the hospital EPR or paper notes
- Starting the initial management plan
Practical point: Clerking forms the backbone of patient care during post-take ward rounds the next morning.
You can also check our complete NHS interview questions guide if you are waiting for your dream job.
Here are some important things you have to make sure are done during the clerking shift:
- Clerking proforma: Make sure this is completed thoroughly. You have put all the bloods, patient details, CXR, ECG, any scans, mentioned or ruled out red flags, your plan, and started any treatment or requested any needed investigations.
- TEP (treatment escalation plan) and DNAR form: This is crucial. Make sure you check this always. If the patient is for full escalation, this is easy. If not, you have to complete DNAR and confirm with the patient that they are happy to continue with DNAR. Make sure you document this clearly (important). If for full escalation and you feel need for DNAR, you can discuss with the patient or NOK if otherwise (lacks capacity) and complete the DNAR form and write the discussion part in the clerking proforma.
- Target location: If you don’t fill it, the A&E staff will be on your head. You have to mention which ward or destination patient is supposed to go from A&E after clerking. This can be a specific ward, say geriatrics or respiratory, or ambulatory or AMU (common) or any procedure room. Make sure you write this in your plan.
- VTE prophylaxis: Most commonly missed by the newcomers. Make sure you complete this and tick this in your clerking proforma.
- Medications: You can look through GP records, previous admissions, shared care portal or sometimes ask the patient or carer or family for this. Make sure it is documented as well as well as put on the system (epma).
![[Guide] NHS On-Call Shifts: What Doctors Actually Do 6 giphy 5](https://i0.wp.com/scrubtales.co.uk/wp-content/uploads/giphy-5.gif?fit=480%2C366&ssl=1)
How much time should I take for clerking a patient?
To answer this question, you have to reflect one simple thing- are you a safe doctor? Well, cut the crap. Normally, if you are new, it takes around 1-1.5 hours to clerk a patient. On a normal 12 hour shift, we usually clerk 8-10 patients.
If you are a team of 4 during a night shift, you will end up clerking around 25-30 patients normally. You can do the maths.
Your job does not ends with clerking the patient, you have to follow up with the crucial tasks as well. This can include ordering urgent investigations, starting treatment, arranging referrals, and most importantly, handing over important tasks to the next team.
If something goes wrong, you have to inform your registrar timely. A good indemnity coverage can help too (no pun intended).
If the patient lands in a ward during or near end of your shift, you will have to hand over these tasks to the ward team, whether it be the on-call ward team or the ward doctors.
Ward Cover Duties
When not clerking, junior doctors on call handle ward cover. This includes:
- Responding to bleeps for issues like chest pain, sepsis, falls, fluid reviews, cannulas, catheters
- Prioritising patient safety — for example, reviewing someone acutely unwell before non-urgent blood test requests
- Documenting all assessments and management
Night Shifts
During night shifts in the NHS, the on-call structure usually remains the same but with fewer staff present. Doctors often:
- Clerk new admissions from A&E or GP referrals
- Cover all wards and step-down units
- Handle emergency calls like cardiac arrests, MET calls, and sepsis alerts
You may find yourself covering multiple wards alone overnight, especially as an FY2 or IMT1. Prioritisation and clear documentation are crucial.
Post-Take Ward Rounds
After night shifts or busy take days, there is usually a consultant-led post-take ward round.
- Doctors present patients they clerked overnight.
- Consultants review each case, update management plans, and sometimes discharge patients.
- Junior doctors update EPR notes and chase outstanding bloods or scans.
Post-take rounds are also where clerking quality is assessed, so getting it right helps both patients and your learning.
Weekend Ward Cover
During weekends, ward cover shifts focus mainly on:
- Reviewing unwell patients already admitted (no routine clerking)
- Handling bleeps for medication reviews, fluids, falls, and patient deterioration
- Prioritising jobs — usually only essential tasks like discharge summaries, reviewing blood results, and responding to emergencies are done
Ward rounds may still happen on Saturdays, often consultant-led but shorter than weekday post-take rounds.
Who covers MET calls and where?
This is another fair question commonly asked and the newcomers have no idea when to respond. Somtimes, they end up in every MET call everywhere, sometimes, they never show.
It’s fairly difficult question to answer as a medic, you are supposed to be in MET call always.
To break it down, if you are a medic doing clerking, you will have to respond to MET calls in wards as well the resus. If you are on-call covering the wards, you will only cover the MET calls in wards.
Furthermore, you will find yourself covering MET calls in theatres sometimes and sometimes in places where you cannot predict. If you are unsure, ask your registrar always.
What if you could not hear where the MET call was? Don’t panic, you can always call switchboard and ask them the answer.
![[Guide] NHS On-Call Shifts: What Doctors Actually Do 7 giphy 6](https://i0.wp.com/scrubtales.co.uk/wp-content/uploads/giphy-6.gif?fit=480%2C362&ssl=1)
Practical Tools and Apps for NHS On-Call Shifts
Managing NHS on-call duties as a junior doctor isn’t just about medical knowledge — knowing which apps and tools to use makes your shift smoother and safer.
If you are still looking for a job, you can try these 5 best places to look for NHS doctor jobs apart from Trac jobs.
Here are the resources I found most useful while working full-time NHS on-call shifts:
Accurx Induction App
The first thing I installed before my first on-call shift was the Induction app. It gives quick access to:
- Bleep numbers
- Hospital switchboard
- Local policies and emergency protocols
It’s essential for navigating ward cover duties, especially if you’re unfamiliar with the hospital layout.
![[Guide] NHS On-Call Shifts: What Doctors Actually Do 8 Accurx Induction Switch App](https://i0.wp.com/scrubtales.co.uk/wp-content/uploads/Accurx-Induction-Switch-App.png?fit=1080%2C1920&ssl=1)
Update: The Induction App has changed to Accurx now.
MicroGuide
During on-call shifts, especially night shifts, doctors often have to prescribe antibiotics without waiting for pharmacy advice. MicroGuide provides:
- Local hospital antimicrobial guidelines
- Dosing advice
- Step-by-step infection management plans
I used it regularly during ward cover and clerking new admissions.
MDCalc or MedCalc
For tasks like clerking patients or reviewing acutely unwell cases, clinical scoring tools come up often:
- Wells score for PE or DVT
- CURB-65 for pneumonia
- HAS-BLED and CHA2DS2-VASc for AF
MDCalc or MedCalc apps are quick, free, and easy to use during busy NHS on-call shifts.
Foundation Doctor Handbook
In my first few months of NHS work, I often checked the Foundation Doctor Handbook during quieter ward cover periods or night shifts.
![[Guide] NHS On-Call Shifts: What Doctors Actually Do 9 Foundation Year Doctor Handbook App](https://i0.wp.com/scrubtales.co.uk/wp-content/uploads/Foundation-Year-Doctor-Handbook-App.png?fit=657%2C1526&ssl=1)
- It’s useful for common on-call scenarios, such as fluid management, sepsis protocols, and escalation guidelines.
- Over time, I found myself relying more on my own MRCP Part 1 knowledge, especially for tasks such as interpreting ABGs or ECGs.
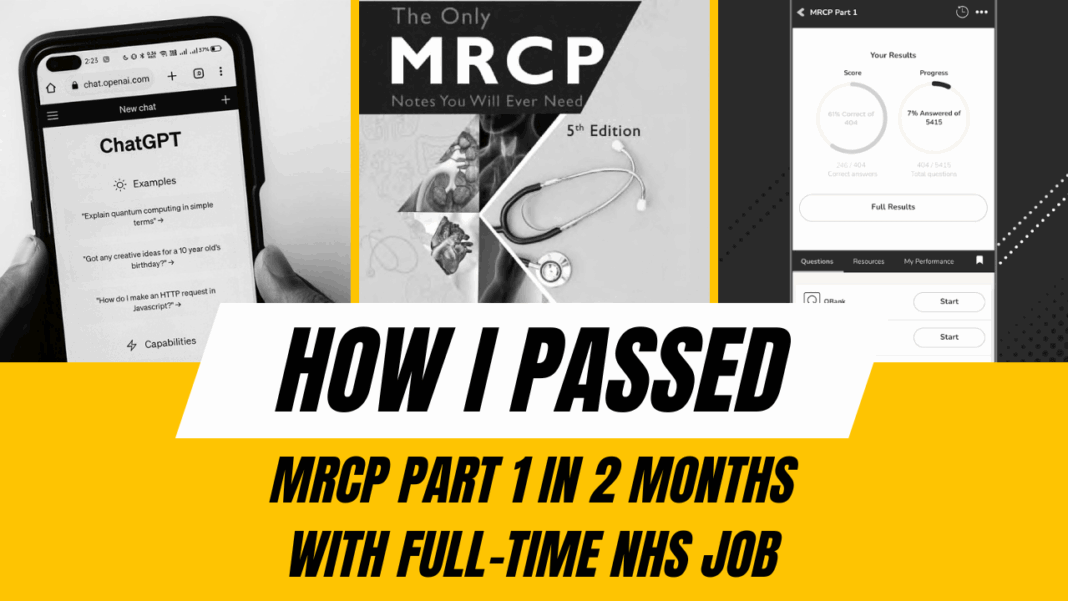
Using ChatGPT for Quick Clarification and Recall Lists
During my MRCP Part 1 preparation, I’d often screenshot tricky Pastest questions and ask ChatGPT for explanations.
- This habit carried over into on-call shifts too: sometimes I’d clarify protocols or management guidelines quickly using ChatGPT.
- I also created personalised recall lists, which I organised on my phone by subject to review between patients.
Remember, the list is not exhaustive and extends to how you personalise your work. Of course, there are other medical apps available that can ease your workload during hectic on-call shifts.
Tips for Doctors Managing NHS On-Call Duties
If you’re an NHS doctor, on-call shifts can feel overwhelming at first. The system, expectations, and escalation protocols may be different from what you’re used to. Here are some realistic tips based on my own experience balancing MRCP Part 1 knowledge and NHS on-call work:
Prioritise Tasks Smartly
During ward cover, you’ll often get several bleeps at once. Learn to prioritise:
- Chest pain, sepsis, or reduced consciousness always come first.
- Routine tasks, such as cannulas or drug charts, can be put on hold if necessary.
Understand UK Escalation Protocols
For NHS on-call shifts, escalation usually follows a clear structure:
- FY1 → SHO → Registrar → Consultant On-Call
- Use SBAR (Situation, Background, Assessment, Recommendation) when handing over or escalating.
- Know when to call your med reg, especially overnight.
Speak Up During Team Introductions
At the start of your on-call shift or early ward round, don’t be shy.
- State your name, grade, and role clearly.
- Make sure others know you’re part of the team and where to find you.
Always Keep Essentials Handy
- Pen and notepad
- Trust ID and bleep
- Phone with Induction and MicroGuide apps installed
- Snacks and water — especially on night shifts!
Rely on Your MRCP Part 1 Knowledge
Doctors often underestimate how much MRCP Part 1 content applies during real NHS on-call duties:
- ECG interpretation
- ABG analysis
- Chest X-ray review
- Clinical scoring systems like CURB-65
While guidelines like the Foundation Doctor Handbook are helpful, your exam revision knowledge fills in gaps when things get busy.
My Final Thoughts on NHS On-Call Duties for Doctors
When I started my first NHS on-call shift as a doctor, I wasn’t sure what to expect. Over time, I realised it’s not just about surviving the rota — it’s about learning how to manage patients safely, work as part of a team, and balance clinical decision-making with real-world NHS protocols.
![[Guide] NHS On-Call Shifts: What Doctors Actually Do 10 giphy 7](https://i0.wp.com/scrubtales.co.uk/wp-content/uploads/giphy-7.gif?fit=480%2C364&ssl=1)
If I could summarise the key takeaways for any new doctor starting NHS on-call duties, they’d be:
- Know your on-call team structure: consultant, registrar, SHOs, FY doctors.
- Focus on key tasks: clerking patients, ward cover, night shifts, and post-take ward rounds.
- Use apps and tools like Induction, MicroGuide, and ChatGPT wisely.
- Rely on MRCP Part 1 knowledge for clinical decision support.
- Always escalate when unsure — patient safety is the top priority.
Even with long nights and stressful moments, NHS on-call shifts are a great learning experience. Each one builds your confidence, sharpens your clinical skills, and helps you settle into working life in the UK healthcare system.